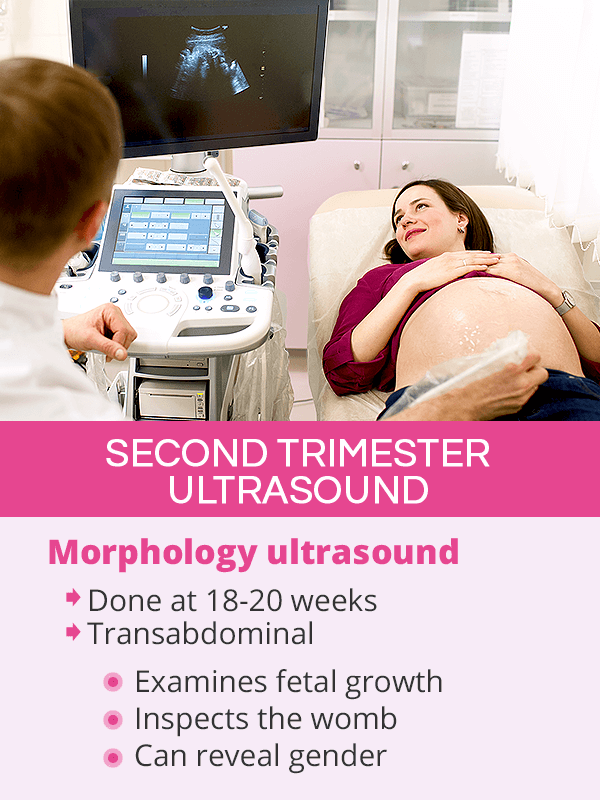
How Many Ultrasounds During Pregnancy are Needed?
Per recommendation of the American College of Obstetricians and Gynecologists (ACOG), healthy, low-risk women with a singleton pregnancy should not routinely get an ultrasound at every prenatal visit. Instead, they are recommended to receive at least one, but not more than two ultrasounds during pregnancy, including a dating scan during the first trimester and a morphology scan during the second trimester1.
However, it has been observed that the exact number of ultrasounds women receive is often higher, depending on the discretion of the OBGYN and a woman's insurance plan, even when not medically indicated.
Additional ultrasounds might be ordered when necessary in the case of twin or triplet pregnancies, complications, or other indications, scenarios which are discussed in the subsequent sections.
Are Ultrasounds Safe for the Baby?
To date, research has not shown evidence that ultrasounds during pregnancy carry any risks for the baby.
However, pregnancy experts discourage using ultrasounds for non-medical reasons, such as keepsake photos of the baby in the womb, as science does not have data on the effects of frequent use of ultrasounds during pregnancy. As such, it is recommended to limit their number to the official guidelines2.
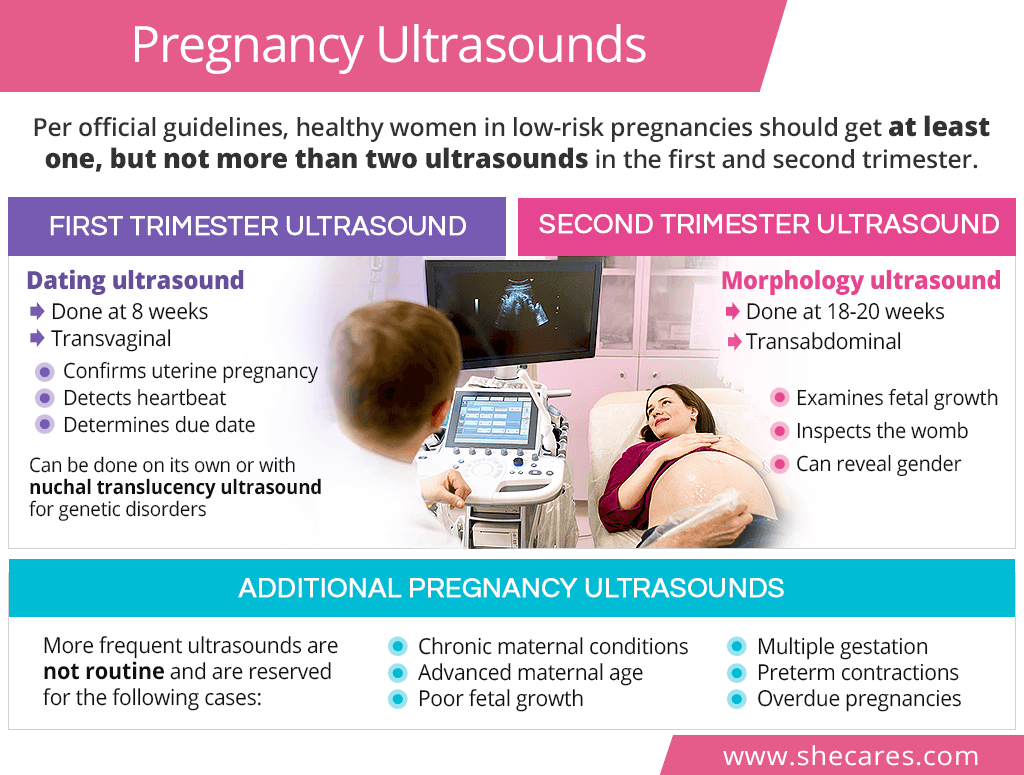
First Trimester Ultrasound
The main first trimester ultrasound is called a dating ultrasound, which can be done alone or combined with a nuchal translucency ultrasound.
Dating Ultrasound
A transvaginal dating ultrasound, or a dating scan, is usually performed at around 8 weeks during the first prenatal visit3. If done after the 10th week, it is generally done transabdominal, instead of transvaginally.
This early pregnancy scan is termed as such because it helps the doctor determine the baby's gestational age and verify whether a woman's estimated due date, which is based on the first day of the last period, is accurate.
Moreover, the first ultrasound during pregnancy is used to confirm pregnancy itself, including identifying initial fetal structures in the uterus, detecting fetal heartbeat, and ruling out ectopic pregnancy. It can also determine whether it is a singleton or a multiple gestation.
Nuchal Translucency Ultrasound
Between the 11th and 14th weeks of pregnancy, a woman might also be offered a transabdominal nuchal translucency ultrasound to evaluate the risk for Down syndrome and other chromosomal defects4. If a dating ultrasound was not done yet, a nuchal translucency can be used for that as well.
It consists of measuring the thickness of the nuchal fold, which is a tissue at the back of the baby's neck. If there is a risk of genetic disorders, this area appears thicker on an ultrasound as more fluid accumulates there. Nuchal translucency ultrasound can be part of the first trimester screening, with the other component being a prenatal blood test called maternal blood serum.
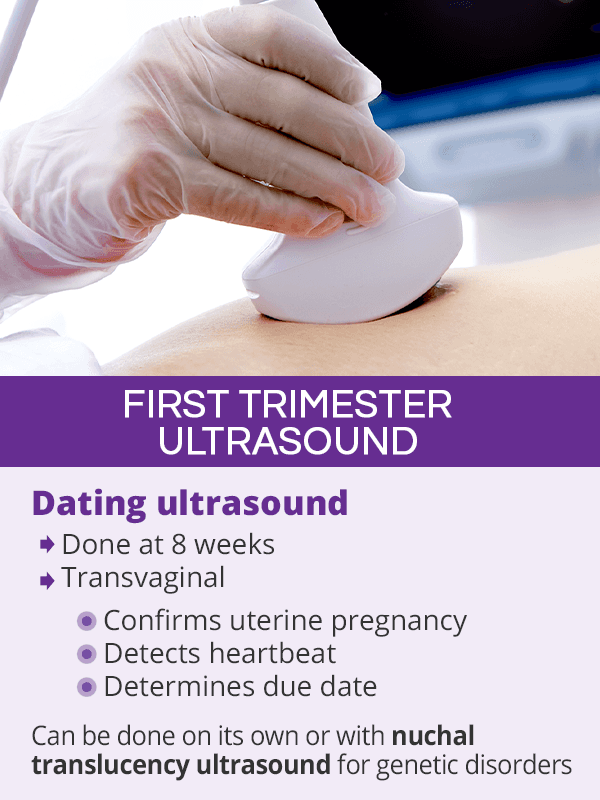
Second Trimester Ultrasound
The second trimester ultrasound is performed between the 18th and 20th week of pregnancy5.
This thorough, transabdominal baby scan is known under several names, including a morphology ultrasound, an anatomy ultrasound, or an anomaly scan. Its purpose is to examine the baby's growth and main organs, like heart, kidneys, or stomach, to promptly recognize any abnormalities. It also inspects the placenta, the umbilical cord, and the levels of amniotic fluid to ensure the baby's well-being.
The scan can also reveal the baby's gender.
Additional Pregnancy Ultrasound
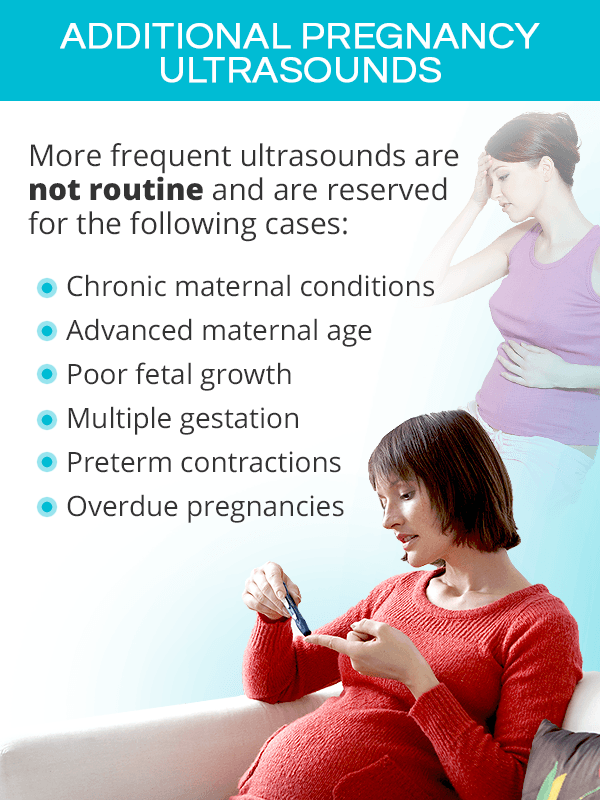
In the case of most normally developing pregnancies, the anomaly scan at 18-20 weeks will oftentimes be the last ultrasound women will receive. As such, a third trimester ultrasound is not a standard part of prenatal testing and its use should be evaluated on a one-to-one basis.
However, more frequent scans or specialized prenatal ultrasounds, like a biophysical profile (BPP), might be ordered throughout all pregnancy stages in the following cases:
- Multiple gestation
- Concerns about fetal growth
- Decreased fetal movement
- Chronic maternal conditions, like high blood pressure, lupus, or diabetes
- Concerns regarding the placenta, amniotic fluid, or the baby's position
- Advanced maternal age
- Preterm contractions
- Vaginal bleeding
- Overdue pregnancies
Key Takeaways
Ultrasounds in pregnancy are an essential tool in ensuring proper fetal growth. However, they are not needed as frequently as many obstetricians-gynecologists are administering them to their patients. Official guidelines state that healthy, low-risk pregnant women in a singleton pregnancy should receive at least one, but not more than two baby ultrasounds. The first one, a dating scan, is done around the 8th week to confirm a uterine pregnancy, detect heartbeat, and estimate due date. It can be done on its own or together with non-invasive genetic testing called nuchal translucency ultrasound. The second recommended baby scan is called a morphology ultrasound, which is done between the 18th and 20th weeks to check on the baby's growth and catch abnormalities soon. Additional ultrasounds should generally be reserved for women in high-risk pregnancies due to advanced age or chronic conditions as well as to evaluate the risk of pregnancy complications, like low amniotic fluid or vaginal bleeding.
Sources
- Beth Israel Deaconess Medical Center. (2018). Ultrasound during Pregnancy: How Many and How Often? Retrieved July 8, 2019 from https://www.bidmc.org/about-bidmc/wellness-insights/pregnancy/2018/09/ultrasounds-during-pregnancy-how-many-and-how-often
- Better Health Channel. (2014). Pregnancy tests - ultrasound. Retrieved July 8, 2019 from https://www.betterhealth.vic.gov.au/health/healthyliving/pregnancy-tests-ultrasound
- March of Dimes. (2014). Ultrasound during pregnancy. Retrieved July 8, 2019 from https://www.marchofdimes.org/pregnancy/ultrasound-during-pregnancy.aspx
- Medline Plus. (2019). Nuchal translucency test. Retrieved July 8, 2019 from https://medlineplus.gov/ency/article/007561.htm
- Medline Plus. (2019). Ultrasound pregnancy. Retrieved July 8, 2019 from https://medlineplus.gov/ency/article/003778.htm
- Office on Women's Health. (2019). Prenatal care and tests. Retrieved July 8, 2019 from https://www.womenshealth.gov/pregnancy/youre-pregnant-now-what/prenatal-care-and-tests
- Seminar in Perinatology. (2013). Benefits and risks of ultrasound in pregnancy. Retrieved July 8, 2019 from https://www.ncbi.nlm.nih.gov/pubmed/24176149
- Wall Street Journal. (2015). Pregnant Women Get More Ultrasounds, Without Clear Medical Need. Retrieved July 8, 2019 from https://www.wsj.com/articles/pregnant-women-get-more-ultrasounds-without-clear-medical-need-1437141219
Footnotes:
- The American College of Obstetricians and Gynecologists. (2014). Fetal Imaging. Retrieved July 8, 2019 from http://www.alabmed.com/uploadfile/2015/0724/20150724095603772.pdf
- FDA. (2014). Avoid Fetal “Keepsake” Images, Heartbeat Monitors. Retrieved July 8, 2019 from https://www.fda.gov/consumers/consumer-updates/avoid-fetal-keepsake-images-heartbeat-monitors
- Pregnancy, Birth & Baby. (2018). Dating scan. Retrieved July 8, 2019 from https://www.pregnancybirthbaby.org.au/dating-scan
- Pregnancy, Birth & Baby. (2018). Nuchal translucency. Retrieved July 8, 2019 from https://www.pregnancybirthbaby.org.au/nuchal-translucency-scan
- Pregnancy, Birth & Baby. (2018). Morphology scan. Retrieved July 8, 2019 from https://www.pregnancybirthbaby.org.au/anomaly-scan