About
Quick Facts about PCOS
- One in every ten women of childbearing age has PCOS.1
- It is said to affect up to 6 million women in the United States.2
- PCOS is one of the most common causes of infertility.2
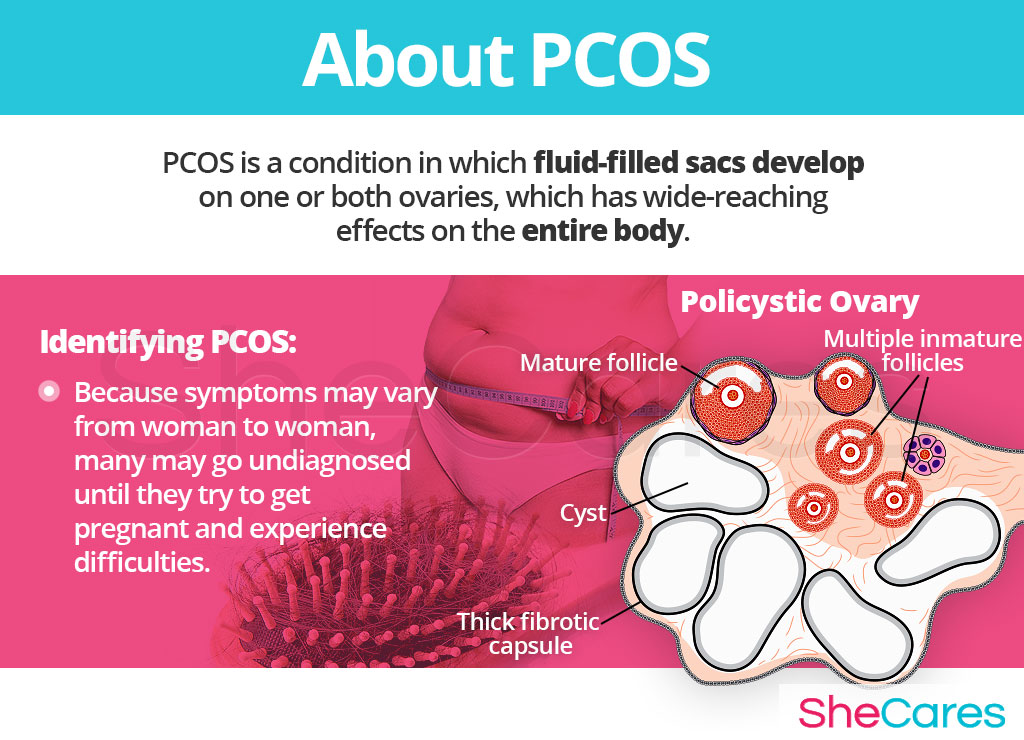
PCOS is classified as a hormonal disorder and characterized by fluid-filled sacs that develop on one or both ovaries.
This condition is closely tied to hormones, particularly an overproduction of androgens, like testosterone.
Identifying PCOS
Identifying PCOS can be tricky as symptoms may vary from woman to woman. As a result, many may go undiagnosed until they try to get pregnant and experience difficulties.
In teens, the symptoms of PCOS may be mistaken with those of puberty, such as acne or menstrual irregularities, among others.
Continue to the next section to discover what causes PCOS.
Causes
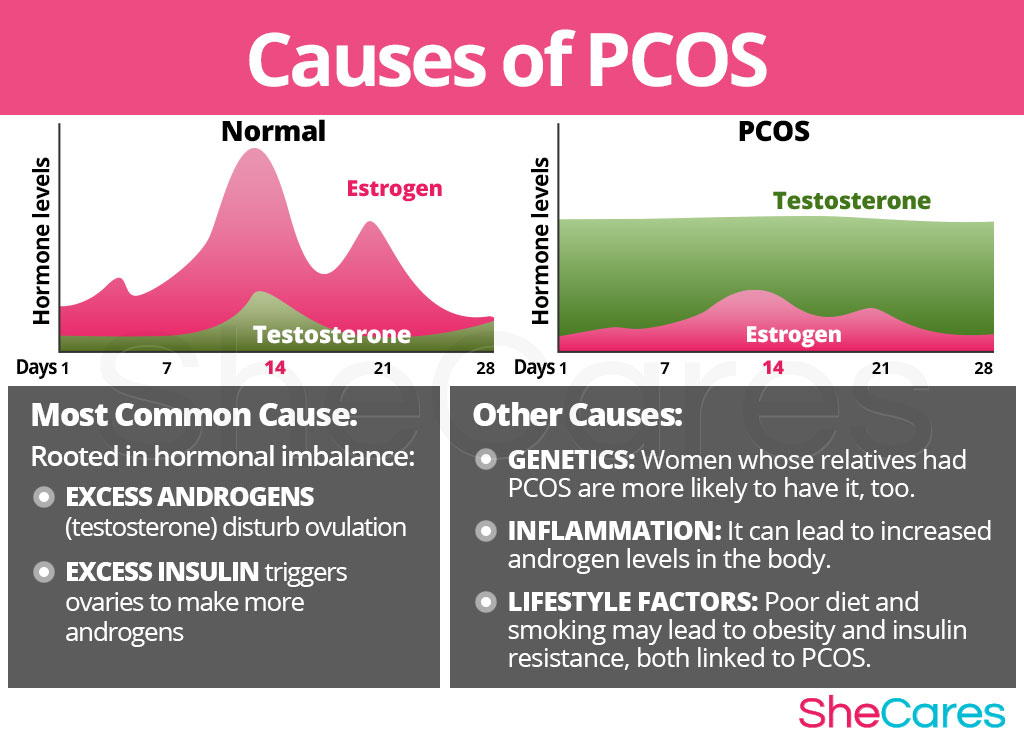
While the exact causes of PCOS are not fully understood, it is believed to have hormonal roots, often in combination with or due to other factors, like genetics.
Hormonal Causes of PCOS
There are two hormonal factors that are of significance when it comes to determining what causes PCOS: high androgen and insulin levels.
Excess Androgens
Androgens is an umbrella term for sex hormones typically associated with males, such as testosterone. Women do produce some androgens, but to a much lesser degree than men.
Excessive androgen levels in PCOS not only cause symptoms like acne and skin growths, but also disturb the development of ovarian follicles and prevent ovulation, thus further worsening the state of hormonal imbalance.
Excess Insulin
Insulin - a pancreatic hormone that influences how the body uses glucose for energy - is also thought to play a role in the development of PCOS.
When a woman's body develops insulin resistance, the levels of glucose and insulin in the blood increase. When not properly managed, excess insulin may trigger the ovaries to make more androgens, thus causing hormonal imbalance and a wide variety of symptoms.
Other Causes of PCOS
Besides hormonal factors, there is strong evidence that genetics play an important role in PCOS as research has shown that women are more likely to suffer from PCOS if their relatives also had it.2
Additionally, various environmental and lifestyle factors, such as poor nutrition or excess body weight, as well as low-grade inflammation may also be potential PCOS causes.3,4 However, more research is needed to corroborate these claims.
Keep reading to learn more about signs and symptoms of PCOS.
Signs and Symptoms
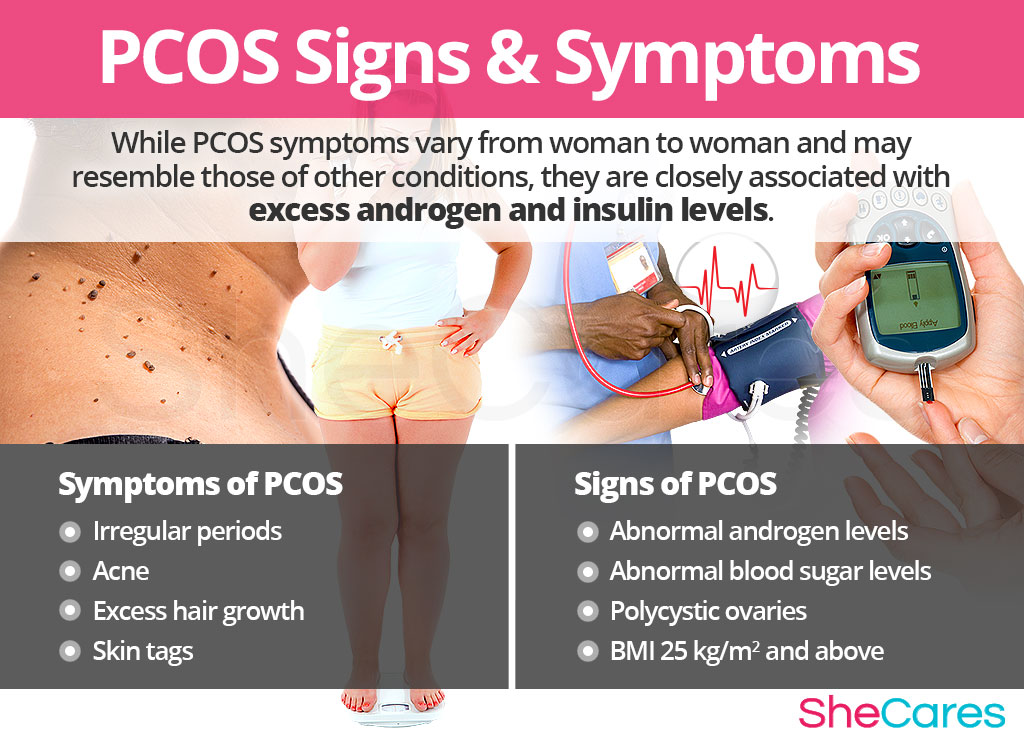
Because symptoms of PCOS vary from woman to woman and may be attributed to other medical conditions, they are not enough to make the final diagnosis. As such, a medical doctor might order diagnostics tests to analyze various signs of PCOS and complete the diagnosis process.
Symptoms of PCOS
While many women notice first PCOS symptoms during puberty, others might not observe any abnormalities until they have trouble getting pregnant later on in life.
When present, most symptoms are closely associated with excess androgen and insulin levels. They may include the following:
- Irregular periods, especially infrequent or absent periods
- Acne
- Excess hair growth, or hirsutism, on the chin, upper lip, chest, or lower abdomen
- Ovulation problems, including anovulation or oligoovulation
- Difficulty getting pregnant
- Darkened skin around the neck and armpits
- Obesity
- Hair thinning on the scalp (male pattern balding)
- Sleep apnea
- Skin tags
Because of excess androgen levels, some women may develop masculine features.
Signs of PCOS
The following are the most characteristic signs of PCOS that will be used in the diagnosis process:
- Abnormal androgen levels
- Abnormal blood sugar levels
- Polycystic ovaries
- Body mass index (BMI) of 25 kg/m2 and above
Diagnosis of PCOS
The signs and symptoms of PCOS can be hard to pinpoint as they may overlap with symptoms of puberty, insulin resistance, diabetes, or other hormonal disorders.
As such, a physician will typically analyze the reported symptoms along with the results of the following medical tests:
Physical exam, including a pelvic exam and a review of the patient's medical history
Blood tests to measure androgen levels as well as other health parameters, like blood glucose or lipids
Ultrasound to confirm the presence of polycystic ovaries
Complications of PCOS
Consistently high hormone levels in PCOS are a recognized risk factor for a number of conditions, most importantly infertility. In fact, PCOS is one of the leading causes of fertility problems among women of reproductive age.7
Those that do manage to get pregnant with PCOS might have higher odds of suffering from gestational diabetes.4
Additionally, women with PCOS might be at an increased risk of obesity and type 2 diabetes, which, in turn, makes them more likely to suffer from cardiovascular problems.8,9,10
A long-term absence of menstruation, or amenorrhea, has also been shown to increase the risk of uterine cancer.10
Continue reading to find out more about the most effective approaches to treating PCOS and restoring your optimal well-being.
Treatments
PCOS treatment is often approached from multiple angles because of the complexity of the condition. The focus is placed on balancing hormones, relieving symptoms, and preventing complications.
Three Approaches to Treating PCOS
There are three levels of approaches that can be considered for treating PCOS, depending on symptom severity and a woman's reproductive plans: (1) Lifestyle Changes, (2) Alternative Medicine, and (3) Conventional Medicine.
Lifestyle changes alongside alternative medicine are generally recommended as the first course of action because they entail the lowest risk and also benefit overall health. For severe symptoms, more conventional and generally more risky options might be more appropriate.
Lifestyle Changes for PCOS
Lifestyle changes are a wholesome approach to treating PCOS. In many cases, the implementation of healthy habits, including eating a nutritious diet, exercising regularly, and reaching a normal weight, may effectively eliminate the symptoms of the condition.
Proper nutrition and physical activity can also enhance a woman's fertility by improving how the body uses insulin and regulating blood glucose levels.
Lifestyle changes can also be safely accompanied by alternative medicine, which is a safe and natural option for balancing hormone levels.
Alternative Medicine for PCOS
While alternative medicine spans a wide range of remedies, herbal supplements in particular can help with PCOS because of the effect they have on hormone levels. Their most common types include phytoestrogenic and hormone-regulating herbal supplements.
Phytoestrogenic herbal supplements
Herbal supplements containing black cohosh, soy, red clover, dong quai, and other herbs are known for their phytoestrogenic content. These plant-based, estrogen-like compounds act like weaker forms of estrogen the body, which can help raise estrogen levels when they are low. While this can assist in balancing the low female sex hormone levels associated with PCOS, it does not directly address excess androgen levels.Hormone-regulating herbal supplements
These supplements, such as Macafem, do not contain any hormones, whether natural or artificial. Instead, they work by stimulating the hormonal glands thanks to the action of their unique alkaloids. The nourishment they provide helps the glands produce sufficient amounts of hormones the body needs, thus promoting overall balance and alleviating PCOS symptoms safely and naturally.Additionally, other herbal supplements may also be beneficial for the treatment of PCOS.
For many women with PCOS, the combination of healthy lifestyle changes and herbal supplements is an effective way to treat the symptoms and balance hormone levels. However, in more severe cases, conventional approaches may be necessary.
Pharmaceutical and Surgical Options for PCOS
While medications for PCOS generally involve more risk, they can effectively balance hormones, alleviate symptoms, and restore ovulation, which may be especially beneficial for women who are trying to get pregnant. They range from combination birth control pills and androgen-blocking medications to ovulation-stimulating drugs and diabetes medication.
Women who want to conceive and did not respond well to lifestyle changes and medications might consider various surgical interventions.
The above approaches can be combined to create a treatment plan that best suits a woman's individual medical needs. While medications for PCOS do show high effectiveness in relieving symptoms and balancing hormones, women oftentimes prefer to rely on natural and side effect-free lifestyle changes and herbal supplements for ultimate relief.

Sources
- Cleveland Clinic. (2015). Your Blood Sugar May Be the Key to Your Hormone Imbalance. Retrieved January 14, 2020 from https://health.clevelandclinic.org/polycystic-ovary-syndrome-pill-not-remedy/
- Harvard Health Publications. (2014). Polycystic Ovary Syndrome. Retrieved March 5, 2017, from http://www.health.harvard.edu/womens-health/polycystic-ovary-syndrome
- International Statistical Classification of Diseases and Related Health Problems 10. (2017). 2017 ICD-10-CM Diagnosis Code E28.2. Retrieved from http://www.icd10data.com/ICD10CM/Codes/E00-E89/E20-E35/E28-/E28.2
- Johnson, N.P. & Wang, K. (2003). Is ovarian surgery effective for androgenic symptoms of polycystic ovarian syndrome? Journal of Obstetrics and Gynaecology, 23(6), 599-606. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/14617458
- Mayo Clinic. (2014). Polycystic ovary syndrome (PCOS). Retrieved March 5, 2017, from http://www.mayo.edu/diseases-conditions/pcos/basics/definition/con-20028841
- Rasgon, N. (2004). The relationship between polycystic ovary syndrome and antiepileptic drugs: a review of the evidence. Journal of Clinical Psychopharmacology, 24(3), 322-334. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/15118487
- Sheehan, M.T. (2004). Polycystic Ovarian Syndrome: Diagnosis and Management. Clinical Medicine & Research, 2(1), 13-27. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1069067/
- UCLA Health. (n.d.). Polycystic Ovary Syndrome (PCOS). Retrieved March 5, 2017, from http://obgyn.ucla.edu/pcos
Footnotes:
- Office on Women's Health. (2016). Polycystic ovary syndrome. Retrieved January 14, 2019 from https://www.womenshealth.gov/a-z-topics/polycystic-ovary-syndrome
- The Endocrine Society. (2018). Polycystic Ovary Syndrome (PCOS). Retrieved January 14, 2020 from https://www.hormone.org/diseases-and-conditions/polycystic-ovary-syndrome
- Steroids. (2012). Inflammation in Polycystic Ovary Syndrome: Underpinning of insulin resistance and ovarian dysfunction. Retrieved January 14, 2020 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3309040/
- Healthy Women. (2019). Polycystic Ovary Syndrome. Retrieved January 14, 2020 from https://www.healthywomen.org/condition/polycystic-ovary-syndrome
- Endocrine. (2006). The role of genes and environment in the etiology of PCOS. Retrieved January 14, 2020 from https://link.springer.com/article/10.1385%2FENDO%3A30%3A1%3A19
- Annals of Indian Academy of neurology. (2016). Polycystic ovary syndrome in patients on antiepileptic drugs. Retrieved January 14, 2020 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4980956/
- ACOG. (2017). Polycystic Ovary Syndrome (PCOS). Retrieved January 14, 2020 from https://www.acog.org/Patients/FAQs/Polycystic-Ovary-Syndrome-PCOS
- John Hopkins M. (n.d.). Polycystic Ovary Syndrome (PCOS). Retrieved January 14, 2020 from https://www.hopkinsmedicine.org/health/conditions-and-diseases/polycystic-ovary-syndrome-pcos
- Obstetrics & Gynecology. (2011). Polycystic Ovary Syndrome and Risk for Long-Term Diabetes and Dyslipidemia. Retrieved January 14, 2020 from https://insights.ovid.com/article/00006250-201101000-00003
- NHS. (2019). Polycystic Ovary Syndrome. Retrieved January 14, 2020 from https://www.nhs.uk/conditions/polycystic-ovary-syndrome-pcos/treatment/
- Clinical Endocrinology. (2012). Vitamin D in the aetiology and management of polycystic ovary syndrome. Retrieved January 14, 2020 from https://www.ncbi.nlm.nih.gov/pubmed/22574874/
- American Journal of Clinical Nutrition. (2012). Effects of increased dietary protein-to-carbohydrate ratios in women with polycystic ovary syndrome. Retrieved January 14, 2020 from https://www.ncbi.nlm.nih.gov/pubmed/22158730
- Gynecological Endocrinology. (2013). Cigarette smoking, nicotine levels and increased risk for metabolic syndrome in women with polycystic ovary syndrome. Retrieved January 14, 2020 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4077900/