What are Birth Control Shots?
Birth control shots are a type of short-lasting, reversible birth control method.
Some women may also be prescribed contraceptive injections for non-contraceptive purposes, including treating irregular periods and relieving menstrual cramps.
In the United States, there is only one approved brand of injectable contraception, called Depo-Provera. For this reason, it is common for a birth control shot to be referred to as the Depo shot.
There is also an alternative version of the shot, called Depo-SubQ Provera 104®, which comes with pre-filled syringes and can be self-administered.
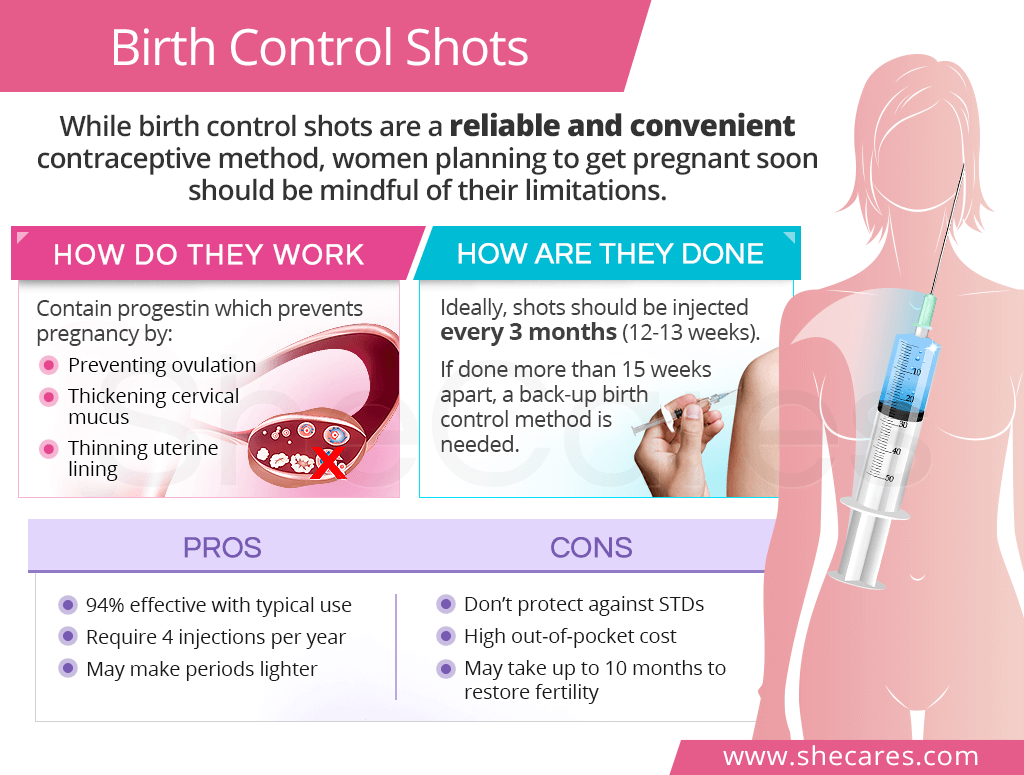
How do Birth Control Shots Work
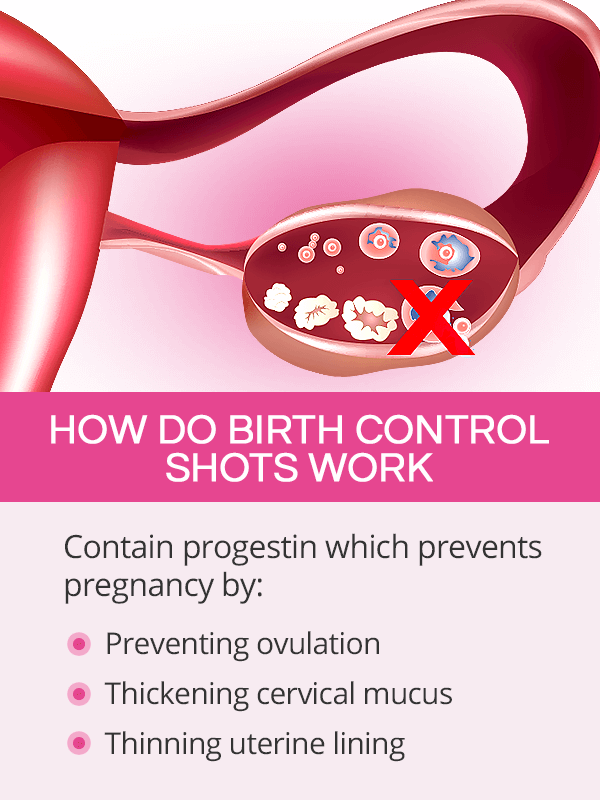
Contraceptive injections contain the hormone progestin, which is a synthetic form of progesterone. A sudden high amount of the hormone causes changes in the body's hormone levels. This, in turn, prevents pregnancy by:
Preventing the egg from being released from the ovary (ovulation)
Thickening cervical mucus so that the sperm cannot get through the reproductive tract to fertilize the egg
Thinning the uterine lining so that the egg would not successfully implant itself
If the injection is done within the first seven days since the beginning of a period, a woman is protected right away. However, if it is administered past seven days since period onset, she should use a back-up contraception for about seven days.1
How Are Birth Control Shots Done
Injectable contraception can be administered in two different ways:

Depo-Provera is injected into the muscle of the upper arm or the buttock. This is typically done by a doctor.
Depo-SubQ Provera 104 is injected beneath the skin in the thighs or abdomen. This can be self-administered.
For birth control shots to effectively prevent pregnancy, they have to be done every three months (12-13 weeks).2
They can be administered as early as 10 weeks since the last shot and as late as 15 weeks since the last shot. If a woman misses her next administration for more than 15 weeks, she should get an additional form of protection for seven days. She may also be given a pregnancy test before the next injection.
Self-administered birth control shots may come with a slightly different administration schedule.3 As such, it is important to clarify it with a doctor to ensure their optimal effectiveness.
Pros and Cons of Birth Control Shots
Although birth control shots have proven to be a reliable and convenient form of preventing pregnancy for thousands of women, they may not be the right fit for everyone.
Birth Control Shots Pros
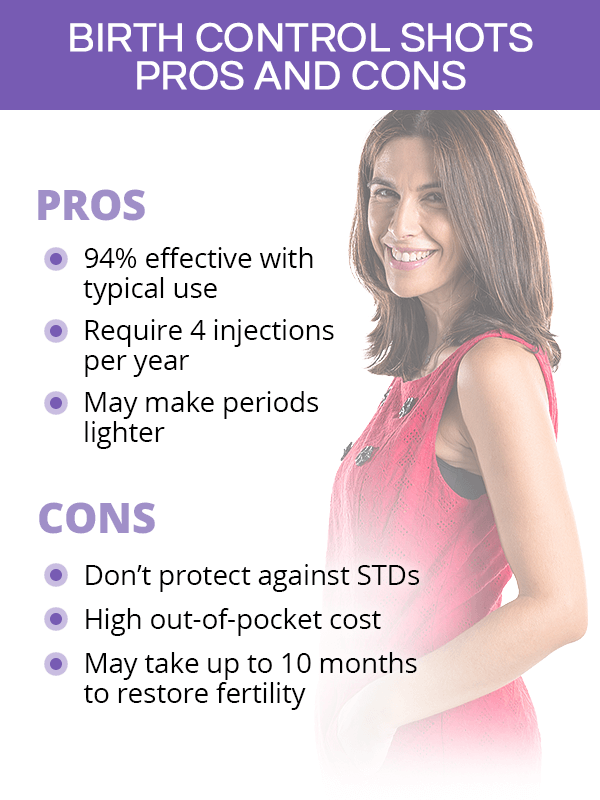
- The shots are more than 99% effective with perfect use and 94% effective with typical use.4
- The shots require only four applications per year, making it easy for women to be compliant.
- The shots can be used by women who cannot or do not want to take estrogen.
- Many women have lighter periods while on birth control shots. After a year, most women stop having periods all together.
- The shots may be self-administered in the skin, which cuts down on doctor's visits and gives women more autonomy.
Birth Control Shots Cons
- Contraceptive injections do not prevent sexually transmitted infections (STDs).
- It may take up to 10 months for a woman's menstrual cycle and fertility to return after stopping the shots.4
- The out-of-pocket cost can be as high as $150 per visit, in addition to doctor's visit fees.
- Studies linked birth control shots to a potentially higher risk of breast cancer in women younger than 35.5
- Long-term use of injectable contraception may affect the amount of calcium in the bones.6
Key Takeaways
Birth control shots are known to give women peace of mind in terms of preventing unplanned pregnancies. They contain progestin which stops ovulation, thickens cervical mucus, and thins the uterine lining so that fertilization and implantation are impeded. The shots come in two different types: one that is done by a doctor and injected into the muscle and another one that comes with pre-filled syringes and can be injected into the skin by a woman. Being on contraceptive injections also requires only four administrations per year, making them a convenient and easier-to-remember option for women. However, birth control shots may delay the return of a woman's periods and fertility for up to 10 months. As such, women who are thinking about becoming pregnant may want to choose another birth control method for the time being.
Sources
- Contraceptive Technology Update. (1992). What is breast cancer risk with Depo-Provera? Received September 14, 2020 from https://pubmed.ncbi.nlm.nih.gov/12343459/
- Mayo Clinic. (2020). Birth control. Retrieved September 14, 2020 from https://www.mayoclinic.org/healthy-lifestyle/birth-control/in-depth/birth-control-options/art-20045571
- Medline Plus. (2020). Birth Control. Retrieved September 14, 2020 from https://medlineplus.gov/birthcontrol.html
- Office on Women's Health. (2017). Birth control methods. Retrieved September 14, 2020 from https://www.womenshealth.gov/a-z-topics/birth-control-methods
- Options for Sexual Health. (n.d.). Birth Control Shot. Retrieved September 14, 2020 from https://www.optionsforsexualhealth.org/facts/birth-control/methods/the-birth-control-shot/
- Women's Health Specialists. (n.d.). Depo Provera Shot. Retrieved September 14, 2020 from Retrieved September 14, 2020 from https://www.womenshealthspecialists.org/services/birth-control/depo-provera-shot/
Footnotes:
- Mayo Clinic. (2020). Depo-Provera (contraceptive injection). Retrieved September 14, 2020 from https://www.mayoclinic.org/tests-procedures/depo-provera/about/pac-20392204
- Planned Parenthood. (n.d.). Birth Control Shot. Retrieved September 14, 2020 from https://www.plannedparenthood.org/learn/birth-control/birth-control-shot
- FDA. (n.d.). Depo-subQ provera 104® medroxyprogesterone acetate injection 104 mg/0.65 mL. Retrieved September 14, 2020 from https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/021583s031lbl.pdf
- Kid's Health. (2018). The Birth Control Shot. Retrieved September 14, 2020 from https://kidshealth.org/en/parents/bc-shot.html
- Family Doctor. (2020). Depo-Provera: An Injectable Contraceptive. Retrieved September 14, 2020 from https://familydoctor.org/depo-provera-an-injectable-contraceptive/
- Cancer Research. (2012). Effect of depo-medroxyprogesterone acetate on breast cancer risk among women 20-44 years of age. Retrieved September 14, 2020 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3328650/