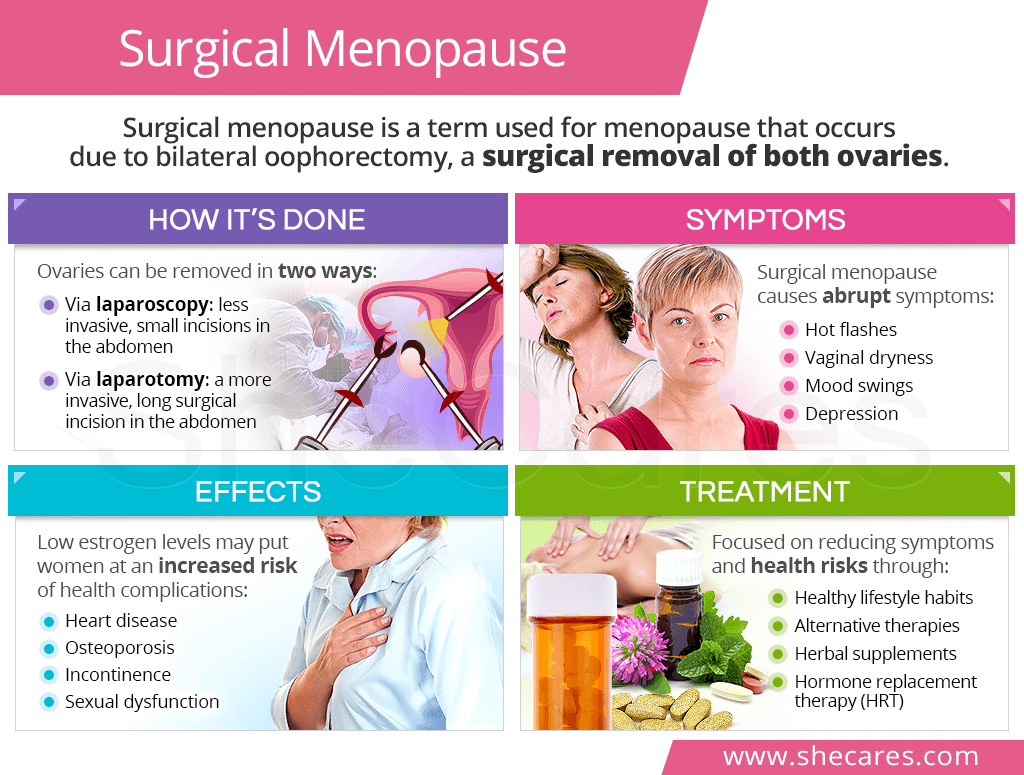
What is Surgical Menopause?
Surgical menopause is a type of induced menopause. The term is used to describe menopause that occurs as a result of a surgical removal of both ovaries, a procedure called bilateral oophorectomy.
Surgical menopause takes place before a woman has reached natural menopause, which normally occurs between the ages of 45 and 55.1 As such:
- If surgical menopause is induced between the ages of 40 and 45, it is considered an early menopause.
- If it is induced before the age of 40, it is considered a premature menopause.2
It is key to differentiate oophorectomy from hysterectomy, which is a surgical removal of the uterus. While both procedures are often done simultaneously, a hysterectomy alone will not trigger immediate menopause since ovaries are left intact.
Reasons to Undergo Surgical Menopause
Surgical menopause is induced mainly for two reasons: either to treat an already diagnosed condition and prevent related complications or to reduce the odds of developing a serious condition in women at high inherited risk.
They include, but are not limited to, the following conditions:
- Endometriosis
- Ovarian cancer
- High risk of ovarian cancer
- Fibroids
- Tubo-ovarian abscesses
- Ovarian torsion
- Benign ovarian tumors
- Recurrent ovarian cysts
While generally reserved as the last resort option, a bilateral oophorectomy is sometimes performed in the following cases:
- Heavy menstrual bleeding (menorrhagia)
- Chronic pelvic pain
- Extreme premenstrual dysphoric disorder (PMDD)
How Is the Procedure Done?
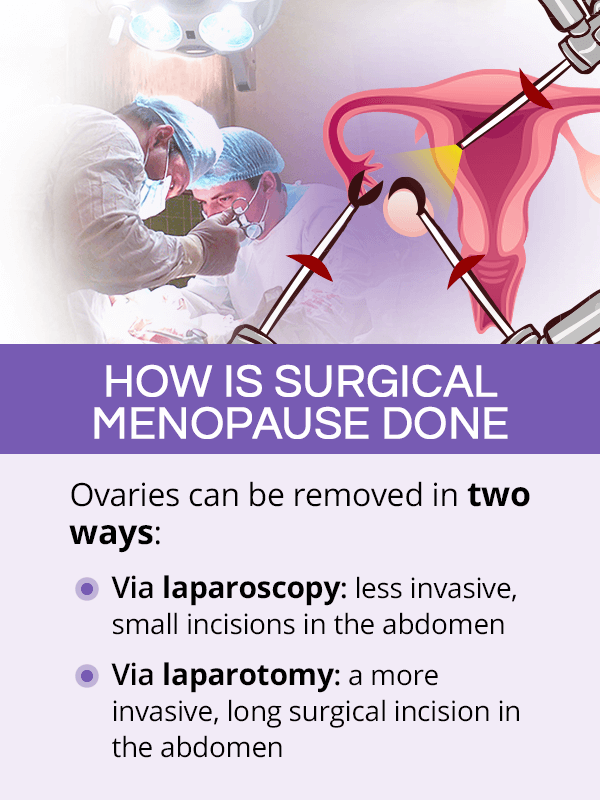
Depending on the underlying reason for a bilateral oophorectomy and other individual factors, the procedure can be done in one of two ways:
Laparoscopy
This minimally invasive technique consists of making small incisions in the abdomen and using instruments to evaluate the abdominal cavity and removing the ovaries. Laparoscopic bilateral oophorectomy has a lower infection risk, and the recovery time is generally shorter.
Laparotomy
This more invasive method involves making a longer incision in the abdomen to remove the ovaries. While still considered a safe procedure, undergoing a bilateral oophorectomy through laparotomy requires a longer recovery time and may come with a higher risk of complications.
Effects of Surgical Menopause
Surgery-induced menopause is known to trigger menopause symptoms right away. It also increases women's risk of developing certain menopause problems in the long-term.
This is because with the removal of both ovaries, the body suddenly loses its main producers of estrogen and progesterone. Estrogen in particular plays a wide range of key roles in the body. As such, its loss can wreak havoc in women's bodies.
Immediate Effects of Surgical Menopause
Besides being sudden, surgical menopause-induced symptoms tend to be more severe than those occurring as part of natural menopause. They include, but are not limited to, the following:
Long-Term Effects of Surgical Menopause
The extent of long-term effects of surgical menopause depends mainly on the age at which it was performed. While estrogen loss affects all menopausal women, having it induced at a younger age comes with an even higher risk of complications, like:
- Osteoporosis and an increased risk of fractures
- Cardiovascular disease after menopause
- Loss of fertility
- Sexual dysfunction and painful sex
- Depression
Surgical Menopause Treatment

Treatment after surgically-induced menopause is mainly oriented towards relieving symptoms of hormonal imbalance that ensues after removing both ovaries.
In younger women, preventing potential complications associated with long-term estrogen lows is also highly important.
Medications
While many women manage their symptoms naturally, some may require pharmacological help for reducing severe symptoms or potential complications. They include the following:
- Hormone replacement therapy (HRT) is nowadays used with caution due to serious side effects linked to its use.3 However, HRT may decrease some health risks in women who undergo surgical menopause at a younger age, as long they do not have contraindications to HRT. Its use, therefore, is evaluated on an individual basis.
- Other medications may also be considered for specific symptoms, such as anti-depressants, sleeping aids, and migraine drugs.
Herbal Supplements
Herbal supplements can be of tremendous help when it comes to easing the effects of hormonal lows and helping women pass through the transition with more ease. Consider the following:
- Phytoestrogenic supplements, such as red clover, contain plant-based estrogens that fill in the hormonal gap, helping alleviate symptoms. To prevent the body from developing a dependency, they are best for short-term use.
- Hormone-regulating supplements, such as Macafem, can be used long-term to nourish the endocrine glands with beneficial alkaloids and stimulate them into improving their own hormone production.
Healthy Lifestyle
After surgical menopause, lifestyle practices should be focused on maintaining bone health, preventing cardiovascular disease, and reducing symptoms at hand. This can be done through:
- Proper nutrition by following a balanced menopause diet with vitamin D, calcium, and phytoestrogens
- Regular exercise that helps maintain a healthy weight, bone health, and balance
- Addiction control, particularly quitting smoking
- Regular doctor's check-ups that monitor lipid levels, blood pressure, glucose levels, and bone density
- Stress reduction and symptom relief through alternative therapies for menopause, like acupuncture or aromatherapy
Key Takeaways
Surgical menopause means that a woman's fertility ends as a consequence of removing both ovaries, a procedure called bilateral oophorectomy. Women may undergo it to treat a condition they already have or prevent a potentially serious condition from developing. Depending on the underlying reason, it can be done either through laparoscopy (less invasive) or laparotomy (more invasive). Because menopause is induced after removing the ovaries, which are the main estrogen producers, sudden and severe symptoms ensue. Long-term estrogen lows also put women at a higher risk of certain health complications. Both symptoms and health risks can be reduced through a variety of approaches, including healthy lifestyle practices, herbal supplements, and medications.
Sources
- Australian Menopause Society. (2017). Surgical Menopause. Retrieved March 11, 2021 from https://www.menopause.org.au/hp/information-sheets/756-surgical-menopause
- BreastCancer.org. (2020). Managing Menopausal Symptoms. Retrieved March 11, 2021 from https://www.breastcancer.org/tips/menopausal
- Cleveland Clinic. (2018). Oophorectomy. Retrieved March 11, 2021 from https://my.clevelandclinic.org/health/treatments/17800-oophorectomy
- International Association for Premenstrual Disorders. (n.d.). Surgery & Surgical Menopause for PMDD/PME. Retrieved March 11, 2021 from https://iapmd.org/surgical-menopause
- Mayo Clinic. (2020). Oophorectomy (ovary removal surgery). Retrieved March 11, 2021 from https://www.mayoclinic.org/tests-procedures/oophorectomy/about/pac-20385030
- Medicine (Kaunas). (2019). Surgically induced menopause- A Practical Review of Literature. Retrieved March 11, 2021 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6722518/
- Menopause. (2007). Surgical menopause and cardiovascular risks. Retrieved March 11, 2021 from https://pubmed.ncbi.nlm.nih.gov/17476145/
- Obstetrics & Gynecology. (2020). Clinical Effects of Early or Surgical Menopause. Retrieved March 11, 2021 from https://journals.lww.com/greenjournal/Abstract/2020/04000/Clinical_Effects_of_Early_or_Surgical_Menopause.15.aspx
- Penn Medicine. (2019). What you need to know about surgical menopause. Retrieved March 11, 2021 from https://www.basser.org/resources/what-you-need-know-about-surgical-menopause
- The North American Menopause Society. (n.d.). Instant Help for Induced Menopause. Retrieved March 11, 2021 from https://www.menopause.org/for-women/menopauseflashes/menopause-symptoms-and-treatments/instant-help-for-induced-menopause
- Women's Health Concern. (2019). Induced menopause in women with endometriosis. Retrieved March 11, 2021 from https://www.womens-health-concern.org/help-and-advice/factsheets/induced-menopause-in-women-with-endometriosis/
Footnotes:
- NHS. (2018). Menopause. Retrieved March 11, 2021 from https://www.nhs.uk/conditions/menopause/
- Cuyuna Regional Medical Center. (2020). Important Information About Early Menopause and Surgical Menopause. Retrieved March 11, 2021 from https://www.cuyunamed.org/wellness/important-information-about-early-menopause-and-surgical-menopause
- The Lancet. (2019). Type and timing of menopausal hormone therapy and breast cancer risk: individual participant meta-analysis of the worldwide epidemiological evidence. Retrieved March 11, 2021 from https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(19)31709-X/fulltext