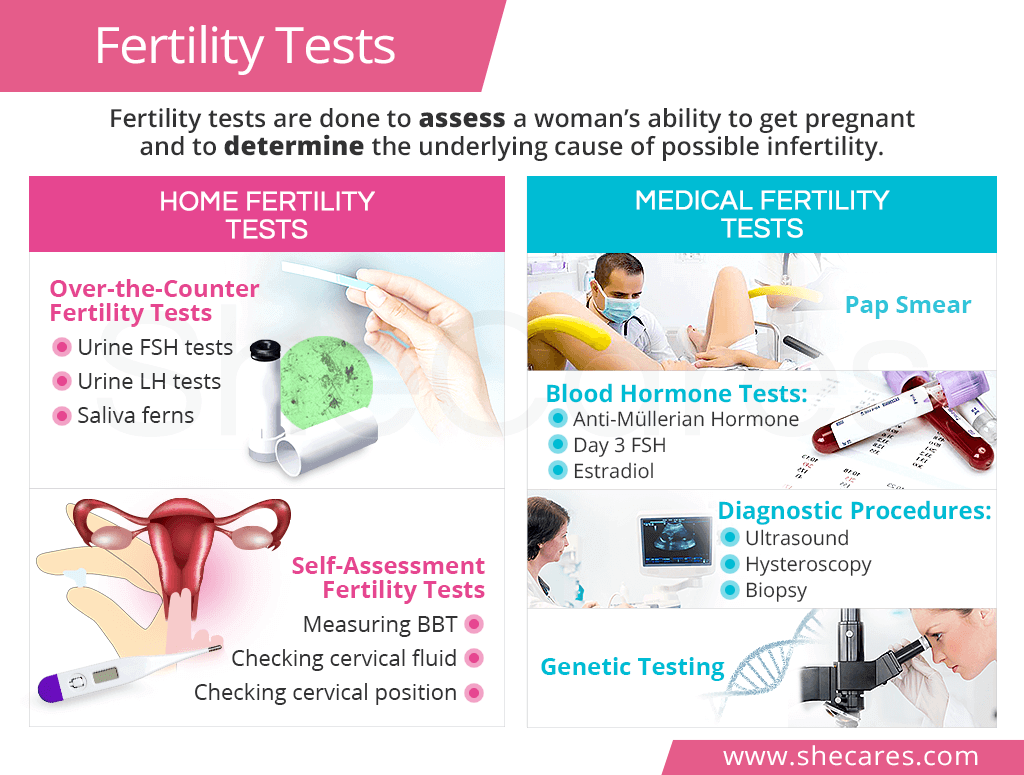
Home Fertility Tests

Because medical fertility tests are recommended after 12 months of trying to conceive, a woman might want to assess her fertility in the meantime with at-home fertility tests.
Since much of female fertility depends on ovulation, most fertility tests done at home revolve around determining ovulatory patterns within a menstrual cycle.
Over-the-Counter Fertility Tests
Ovulation test kits detect hormonal levels around ovulation, including luteinizing-hormone (LH) or follicle-stimulating hormone (FSH). Low LH right before ovulation or high FSH on the third day of the cycle indicate ovulation problems.
Ovulation microscopes enable a woman to do a quick fertility check by identifying ferning patterns in the saliva or cervical mucus, which occur due to rising estrogen before ovulation. The absence of ferns can indicate a potential fertility problem.
Self-Assessment Fertility Tests
Measuring basal body temperature is one of the most common home fertility tests. A lack of the progesterone-triggered temperature spike means that ovulation does not occur.
Checking cervical mucus for its egg-white consistency can help determine if ovulation is approaching. However, this home fertility test might not be effective for all women as some are not able to trace those vaginal changes.
Checking cervical position can also serve as a female fertility test as the cervix moves higher up into the body and becomes soft and open as ovulation is near.
Collecting the results of the aforementioned home fertility tests along with menstrual patterns will be very useful during a consultation with the OBGYN or a fertility specialist.
Medical Fertility Tests
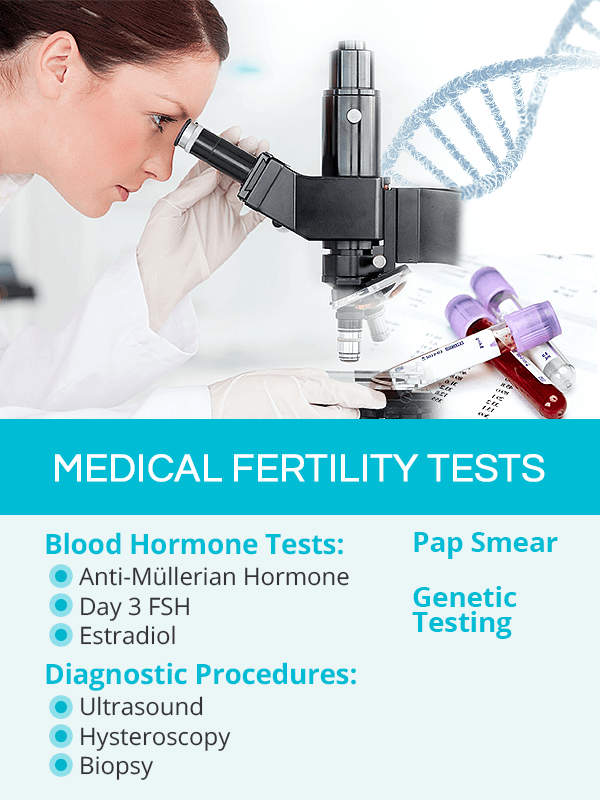
Medical fertility tests are a part of the diagnostic work-up for infertility treatment or evaluations for fertility preservation.
Each fertility evaluation should start with proper gynecological consultation, during which the doctor will review a woman's medical history, including menstrual patterns, and perform a physical exam.
Based on the collected information, he or she might order one or several fertility tests:
Pap Smear
It is a standard gynecological procedure consisting of taking samples of cells from the surface of the cervix. It can show cervical problems or undiagnosed sexually transmitted diseases (STDs) that can cause fertility problems.
Blood Tests
Because most fertility problems are rooted in hormonal imbalance, a standard doctor's work-up will include a comprehensive screening of hormone levels. Fertility blood tests can check if ovulation is occurring, rule out other underlying endocrine disorders, and verify the state of the ovarian reserve, particularly the egg count.
Anti-Müllerian Hormone (AMH) is the most common egg count blood test. The hormone is produced by the developing ovarian follicles. Low AMH levels signal low egg count as the cause of fertility problems.
Day 3 FSH blood test checks follicle-stimulating hormone levels, which in the beginning of the cycle, should be low. High FSH levels on day 3 indicate that ovulation might not be occurring properly. Another variation of an FSH test is done in combination with timed administration of the fertility medication clomiphene citrate for more accurate results.
Estradiol (a form of estrogen) blood test verifies if the hormone is rising in the first part of the cycle as it is produced by the follicles. Low estradiol levels mean low ovarian reserve.
Other standard blood tests might include a complete blood count (CBC), comprehensive metabolic panel (CMP), and thyroid hormone levels (TSH, T4, T3), all of which will provide insight of a woman's overall health status.
Diagnostic Examinations
Infertility investigations typically start with a transvaginal ultrasound, which along with the AMH lab test, is the most common fertility test. Other diagnostic procedures are added as necessary to reach a final diagnosis.
Transvaginal ultrasound is used to perform an egg count test called the antral follicle count, which gives view of the number of ovarian follicles that were recruited for maturation. It helps determine if fertility issues are due to low ovarian reserve. Through an ultrasound, a doctor can also check for anatomical abnormalities in the uterus and ovaries that might be the culprit of infertility.
Hysterosalpingogram (HSG) is a test during which a dye is injected through the cervix, and a series of X-rays is taken to locate blockage or damage to the reproductive organs that might prevent pregnancy.
Hysteroscopy is a follow-up procedure when some abnormalities were found with HSG. It is done by inserting a scope with a camera into the uterus to provide a clear view of possible scarring, blockage, or other problems, such as endometriosis or PCOS.
Laparoscopy is similar to a hysteroscopy with the exception that if abnormal growth or scarring is found during a laparoscopy, it can be immediately removed. This procedure is done under general anesthesia.
Endometrial biopsy is done to ensure that the endometrial lining's thickness is sufficient to support a fertilized egg and the fetus. It consists of taking a sample of the endometrium right before a woman's period.
Genetic Testing
Genetic testing is recommended for couples when aforementioned tests do not provide enough clues about the underlying reason for their infertility. Because DNA issues account for up to 10% of infertility problems, the testing needs to be done on both partners.
Male Fertility Tests
Male infertility accounts for about 50% of fertility problems. It is, therefore, crucial for male partners to undergo proper testing as well.
Male fertility tests may include a physical exam of the genitals; semen analysis to check sperm count, shape, and mobility; and blood tests for STDs, anti-sperm antibodies, and hormone levels, especially testosterone.
Additional fertility tests for men might comprise of post-ejaculation urinalyses, scrotal or transrectal ultrasounds, and a testicular biopsy, among others.
Key Takeaways
A fertility test for women can be taken at home or at a medical facility. Home fertility tests help women assess their ability to conceive and focus on monitoring ovulatory patterns through checking urine hormone levels or measuring BBT. Medical fertility tests, on the other hand, are recommended to couples after failing to get pregnant after 12 months of trying. They are a part of infertility investigations and might include a pap smear for STDs and cervical problems; blood tests to rule out hormonal imbalance; diagnostic procedures to detect abnormalities of the reproductive organs; or genetic testing for DNA defects causing fertility problems. Male partners should also undergo appropriate fertility tests alongside women for optimal conception success.
Sources
- American Pregnancy Association. (2018). Female Fertility Testing. Retrieved October 12, 2018 from http://americanpregnancy.org/infertility/female-fertility-testing/
- CDC. (2018). Infertility FAQs. Retrieved October 12, 2018 from https://www.cdc.gov/reproductivehealth/infertility/index.htm
- Current Urology Reports. (2011). Use of Diagnostic Testing to Detect Infertility. Retrieved October 12, 2018 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3079371/
- Mayo Clinic. (n.d.). Infertility. Retrieved October 12, 2018 from https://www.mayoclinic.org/diseases-conditions/infertility/diagnosis-treatment/drc-20354322
- Medline Plus. (2018). Infertility. Retrieved October 12, 2018 from https://medlineplus.gov/infertility.html
- Office on Woman's Health. (2018). Trying to conceive. Retrieved October 12, 2018 from https://www.womenshealth.gov/pregnancy/you-get-pregnant/trying-conceive