About
Quick Facts about Dyspareunia
- The most common sexual difficulties experienced by women around menopause include dyspareunia, loss of sexual interest, and arousal difficulties.
- About 25 - 45% of postmenopausal women find sex painful.
- Dyspareunia affects 8 - 22% of females, making it a very frequent issue in gynecologic practice.
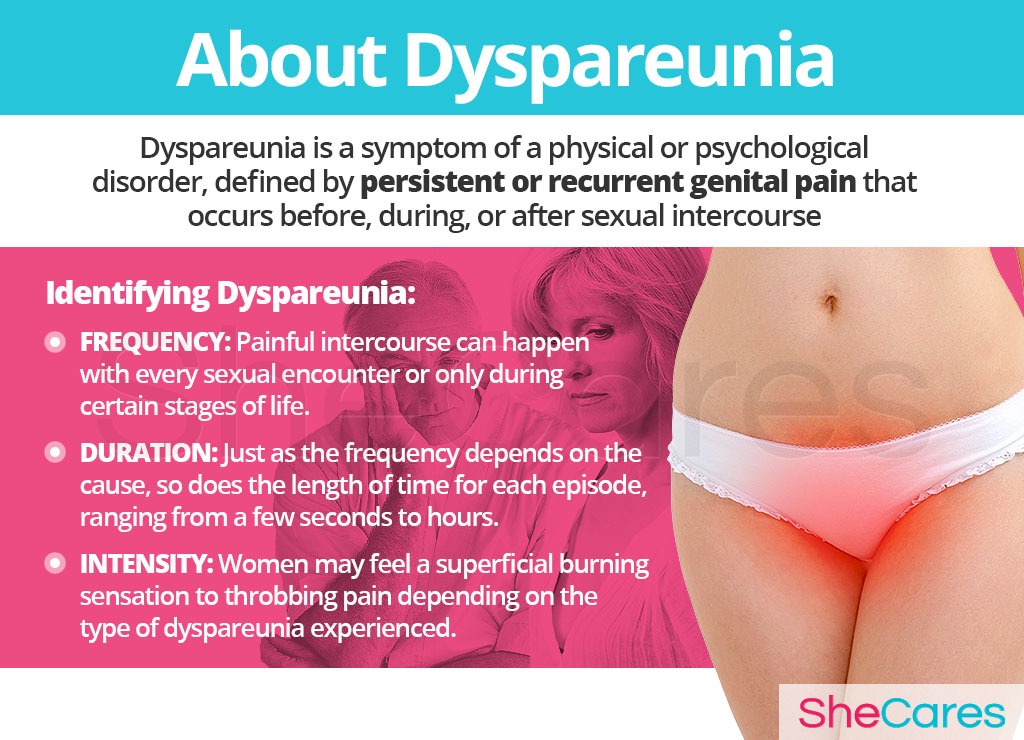
First off, it is important to note that dyspareunia is not a disease, but a symptom of a physical or psychological disorder. All cases can be grouped into superficial dyspareunia or collision dyspareunia.
Moreover, there are two, generally accepted types of dyspareunia: primary and secondary. Primary dyspareunia is the classification of dyspareunia in which pain has always occurred during sexual activity. On the other hand, secondary dyspareunia is where the pain begins to occur after a period of pain-free intercourse.
Identifying Dyspareunia
Accurately establishing the specific types and causes of dyspareunia can be challenging as they vary drastically from woman to woman. However, there are three criteria that can help identify dyspareunia and ways in which it varies: frequency, duration, and intensity.
Causes
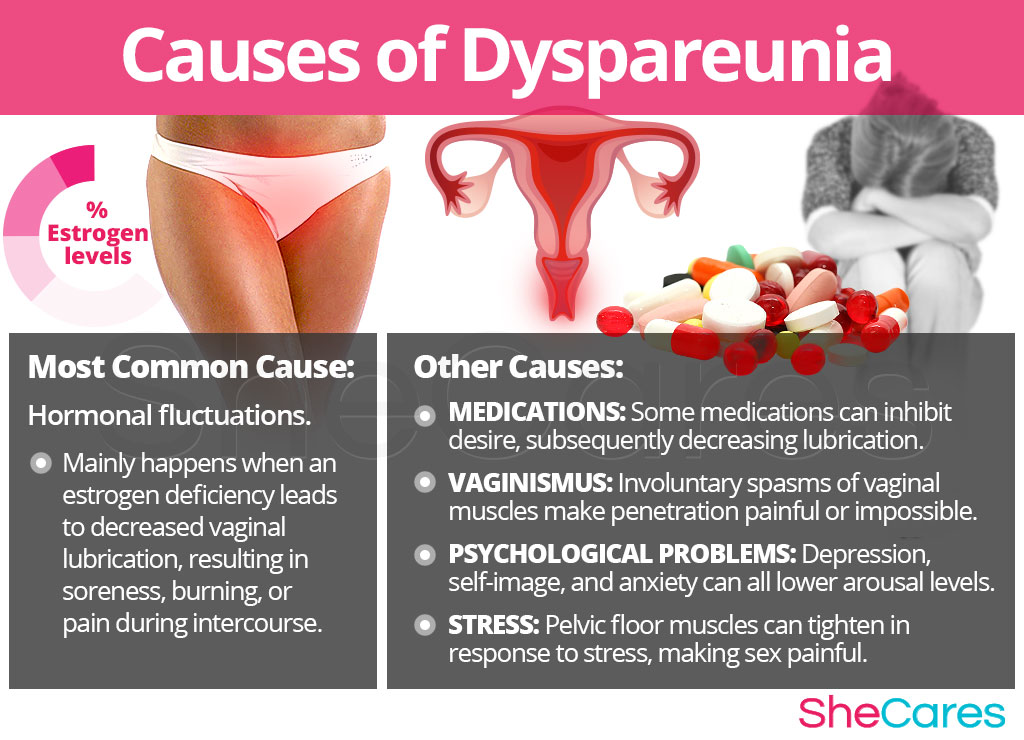
Dyspareunia can be caused by a variety of physical or psychological problems, making it difficult to pinpoint the exact cause of the symptom.
Familiarizing oneself about the main hormonal cause of dyspareunia allows for better understanding into how to manage and treat the condition.
Main Cause of Dyspareunia: Hormonal Fluctuations affecting Vaginal Lubrication
In general, estrogen hormones, produced by women's ovaries, are responsible for maintaining the elasticity and health of genital tissues, controlling the vagina's ability to expand, contract, and grow to new cells.
An estrogen deficiency leads to decreased secretion of lubricant, resulting in various unpleasant aftereffects to sex, such as soreness, burning after sex, pain during intercourse, and post-sex bleeding. Declining levels of estrogen also increase tissue fragility and the probability of vaginal tissue trauma.
There are several stages within a woman's reproductive life in which it will be more likely for her to have dyspareunia, including postpartum, breastfeeding, perimenopause, postmenopause, and even PMS.
Other Causes of Dyspareunia
The cause of this symptom in a given person may be a combination of several factors, and in some cases, the precise cause may not be identifiable at all. Other causes of dyspareunia include medications; conditions such as vaginismus, endometriosis, and vulvovaginal atrophy; and emotional factors such as stress and sexual abuse.
Risk Factors and Triggers
Risk Factors for Dyspareunia
Risk factors for dyspareunia are characteristics that serve as potential reasons for women to have dyspareunia. Just because a woman may have several risk factors does not mean that she will automatically experience painful sex. Once a woman is officially diagnosed, doctors will decipher the ultimate cause, determining if a risk factor for dyspareunia was to blame.
Some women are more likely than others to experience dyspareunia because of health and behavioral risk factors. Health risk factors include menopausal age, untreated sexually transmitted diseases (STDs), and medical conditions, including endometriosis. Behavioral risk factors include lack of proper hygiene and practicing unprotected sex.
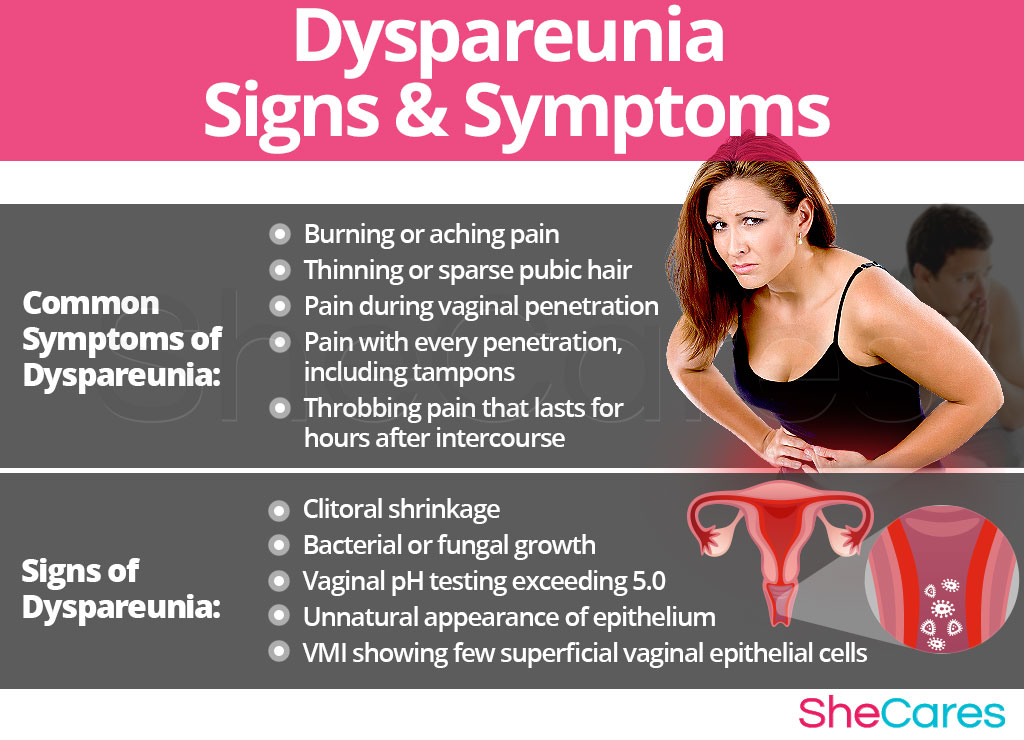
Signs and Symptoms
Women experience dyspareunia symptoms and discomfort of varying degrees, depending on if the disorder is superficial, vaginal, or deep.
Common Symptoms of Dyspareunia
- Burning or aching pain
- Thinning or sparse pubic hair
- Throbbing pain that lasts for hours after intercourse
- Pain during vaginal penetration (upon entry or with thrusting)
- Pain with every penetration, including tampons (could indicate vaginismus)
Signs of Dyspareunia
As opposed to more noticeable symptoms, medical signs are measurable criteria that are usually assessed by a physician. The following medical signs will most likely be taken into account by a physician when diagnosing dyspareunia, especially when caused by vulvovaginal atrophy.
- Clitoral shrinkage
- Vaginal pH testing exceeding 5.0 (signifies estrogen deficiency)
- Bacterial or fungal growth (shown by microscopy)
- Vaginal maturation index (VMI) showing few superficial vaginal epithelial cells
- Appearance of hypo-pigmented, smooth, non-elastic, thin and/or shiny epithelium
Diagnosis of Dyspareunia
To diagnose and identify the symptoms of dyspareunia, a doctor must typically perform several procedures. First, he or she will review the patient's medical history, conduct a physical exam, and finally do some testing. The doctor may order additional tests if necessary.
Complications of Dyspareunia
Dyspareunia does not usually bring about major health complications. More often than not, it will just affect the sex lives of those who have it. Avoiding treatment will just prolong the suffering.
However, there are certain changes women can consider to prevent experiencing dyspareunia depending on its cause, and women already experiencing dyspareunia would benefit from learning how to manage or treat the condition.
Prevention and Management
Preventing Dyspareunia
In many cases, dyspareunia cannot be prevented, especially if due to psychological problems and the result of surgeries or traumas.
However, there are a few steps perimenopausal or postmenopausal women can take to keep their hormone levels balanced and reduce the risk of experiencing dyspareunia due to insufficient estrogen levels.
Lifestyle Changes for Prevention
- Nutrition. By eating a balanced diet rich in fresh fruits and vegetables with healthy phytoestrogenic sources - such as beans, alfalfa sprouts, and flaxseed - to correct hormonal imbalances, it is possible to begin the preliminary steps of preventing dyspareunia.
- Exercise. Regular exercise is important to maintain a healthy body weight, but depending on the severity of a woman's irritation around the vaginal area, vigorous exercises may or may not help with dyspareunia. If the condition is caused by vaginismus, yoga stretching immediately before intercourse may help relieve muscular tightness. Deep breathing and relaxation through yoga also help relieve stress for a higher level of well-being and an improved self-image. Moreover, contraction-relaxation exercises to improve the pelvic floor may be added in a routine.
- Healthy habits. It is important to limit alcohol consumption and quit smoking as it causes the body is produce less estrogen, the hormone that maintains elasticity and health of genital tissues. It is also important to practice good hygiene to avoid the risk of infection. Habits like wiping from front to back, urinating after sexual intercourse, showering regularly, and changing undergarments after prolonged sweating all help.
Managing Dyspareunia
In whichever life stage a woman finds herself when diagnosed with dyspareunia, there are effective methods for management of dyspareunia, especially in regard to steps the couple can take during sexual intercourse to ease the discomfort. Making minor changes can make a huge difference for women who are trying to overcome dyspareunia.
Moreover, there are certain tips to follow that can help improve the sexual experience on behalf of the women, giving her stepping stones she needs to cope. The following are general management tips for dyspareunia that women of all ages can use, such as using lubrication, finding other ways to be intimate, and communicating more.
Alternative Management Tips for Dyspareunia
Alternative treatments can also be a useful way to manage dyspareunia. These treatments will not tackle the hormonal cause behind most women's sexual discomfort, but they are effective in helping the woman overcome physical discomfort and relationship stress. Alternative treatments include desensitization therapy, couple counseling, and cognitive behavior therapy.
While these measures often help women learn how to better manage and prevent the initial onslaught of dyspareunia, they do not directly target the underlying cause of many women's dyspareunia, hormonal imbalance. However, there are several natural dyspareunia treatments that can help bring reproductive hormones back to healthy levels.

Treatments
Treating dyspareunia not only improves a woman's sex life, but it also will improve her self-image and emotional intimacy with her partner.
Three Approaches to Treat Dyspareunia
Three levels of approaches can be considered for treating dyspareunia depending on the underlying cause. These are categorized as: (1) Lifestyle Changes, (2) Alternative Medicine, and (3) Pharmaceutical Options.
Depending on the condition, medical intervention may be necessary for dyspareunia treatment. The cause of dyspareunia will also influence the duration of treatment. For example, treatment of dyspareunia caused by urinary tract or yeast infections usually takes within a week while dyspareunia solely caused by inadequate lubrication can be improved rapidly with lubricant or proper arousal.
If possible, women are encouraged to begin with the least risky approach, lifestyle adjustments, and then proceed to the next level of care based on their specific situation.
Lifestyle Changes
This primary level of dyspareunia treatment involves the least amount of risk; although, it conversely requires the highest amount of self-discipline. Often, simple changes in lifestyle can reap huge benefits in achieving a higher overall level of health. Fundamentally, start with an improved diet, regular exercise, and healthy habits.
Although these changes will help promote over well-being, they are often not the most direct way to balance insufficient estrogen levels, one of the leading causes of dyspareunia in older women. Further treatment may be necessary. Alternative medicine has proven to be an excellent way of preventing dyspareunia related to hormonal imbalance in a safe and natural way.
Alternative Medicine for Dyspareunia
Alternative medicines and supplements generally involve little to no risk and can be an extremely effective for preventing and treating dyspareunia in its entirety, depending on the initial cause. In the case of herbal supplements, there are two main types to take into consideration: phytoestrogenic and hormone-regulating herbal supplements.
Phytoestrogenic herbal supplements
Similar to the phytoestrogenic foods, these supplements, such as chaste berry, contain estrogenic components produced by plants that help regulate hormones. By taking plant-based estrogens, women can maintain higher estrogen levels to prevent or stop dyspareunia. Sufficient amounts of estrogen will maintain the elasticity and health of genital tissues by also providing adequate vaginal lubrication.
Hormone-regulating herbal supplements
These non-estrogenic supplements, including Macafem, stimulate the endocrine system and treat underlying hormonal imbalances. By stimulating natural hormone production, these supplements promote healthy estrogen levels to ultimately prevent or stop the effects of dyspareunia. They can be taken throughout a woman's life as they trigger natural hormonal development instead of artificial replacement.
Additionally, there are other types of supplements that promote a healthy hormonal balance, including soy protein.
A combination of approaches is usually the most effective route to take. Lifestyle changes combined with alternative medicine can ultimately help a woman overcome dyspareunia caused by hormonal imbalances. However, for some women, dyspareunia will be so severe that a more drastic treatment is necessary.
Pharmaceutical Options for Dyspareunia
Interventions at the third level involve the highest risk and often the highest costs. Not all treatments are suitable for women at every life stage; therefore, it is strongly recommended to speak to a licensed healthcare practitioner before starting any pharmaceutical dyspareunia treatment.
Consequently, there are no specific medications used to cure dyspareunia as medicinal treatment is based on the underlying condition. It is important to note that use of certain prior medications can actually cause problems in lubrication, and elimination of these drugs will solve symptoms and the problem of painful intercourse.
Without a doubt, the main type of pharmaceutical option prescribed to treat dyspareunia in perimenopausal and postmenopausal women, specifically, is HRT. For all women in general, other artificial estrogen products and over-the-counter lubricants can help with dyspareunia.
Overall, these three approaches are not mutually exclusive. A woman may use different approaches at different times or any combination of them, depending on her specific situation. Recently, more and more women find that preventing and dealing with dyspareunia can be accomplished via a combination of healthy lifestyle and alternative treatments.

Sources
- American College of Obstetricians and Gynecologists. (2009). Evaluation and Treatment of Dyspareunia. Retrieved May 25, 2017, from https://www.med.unc.edu/ppru/publications/Evaluation%20and%20treatment%20of%20dyspareunia.pdf
- Australian Family Physician. (2011). Sex and perimenopause. Retrieved May 24, 2017, from http://www.racgp.org.au/download/documents/AFP/2011/May/201105davis.pdf
- Harvard Health Publications. (2013). Painful Sexual Intercourse (Dyspareunia). Retrieved May 25, 2017, from http://www.health.harvard.edu/womens-health/painful-sexual-intercourse-dyspareunia
- International Journal of Women's Health. (2009). Treating dyspareunia caused by vaginal atrophy: a review of treatment options using vaginal estrogen therapy. Retrieved May 24, 2017, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2971714/
- Mayo Clinic. (n.d.). Painful intercourse (dyspareunia). Retrieved May 22, 2017, from http://www.mayoclinic.org/diseases-conditions/painful-intercourse/basics/definition/con-20033293
- National Women's Health Resource Center. (n.d.). When Sex Hurts. Retrieved May 25, 2017, from http://www.healthywomen.org/content/article/when-sex-hurts
- The Obstetrician & Gynecologist. (2005). Dyspareunia following childbirth. Retrieved May 24, 2017, from http://onlinelibrary.wiley.com/doi/10.1576/toag.7.4.245.27119/pdf
- Oman Medical Journal. (2017). Treatment of Vaginal Atrophy with Vaginal Estrogen Cream in Menopausal Indian Women. Retrieved May 24, 2017, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5187400/
- Pain Research and Management. (2008). Dyspareunia in postmenopausal women: A critical review. Retrieved May 25, 2017, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2671314/
- Women's Health Concern. (n.d.). Vaginal dryness. Retrieved May 31, 2017, from https://www.womens-health-concern.org/help-and-advice/factsheets/focus-series/vaginal-dryness/