About
Quick Facts about Osteoporosis
- Studies suggest that approximately one in two women age 50 and older will break a bone due to osteoporosis.
- Peak bone mass is achieved around age 30.
- During the first five years of menopause, the average woman loses up to 10% of her total bone mass.
Bones are in a constant state of renewal as they are being broken down and replaced. As new bone is made, old bone is broken down. Most people reach their peak bone mass by their early 20s because younger bodies make new bones faster than they break down old bones.
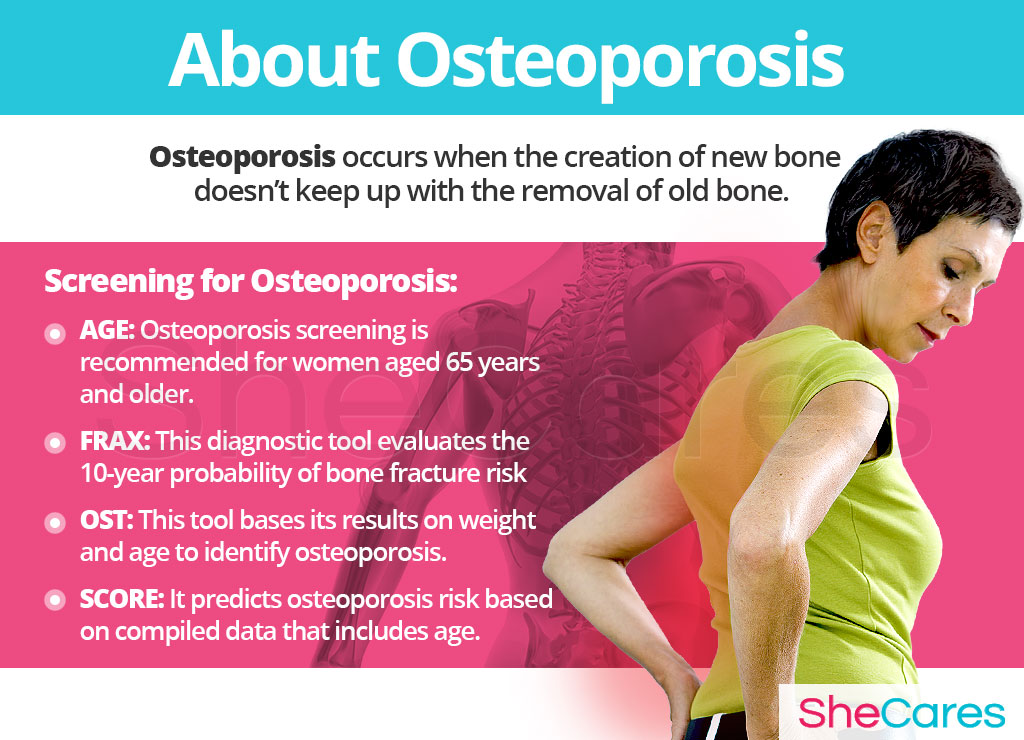
As people age, bone mass is lost faster than it's created. Subsequently, osteoporosis occurs when the creation of new bone doesn't keep up with the removal of old bone.
Osteopenia is considered by many to be a precursor to osteoporosis, as it is reduced bone mass of lesser severity than osteoporosis. This decreased bone density leads to fragility and an increased chance of fracture.
Identifying Osteoporosis
Only 1 in 3 patients with osteoporosis is diagnosed. Therefore, helping identify those who are candidates to receive a bone mineral density (BMD) test for osteoporosis screening is the important first step. There are several criteria and tools used to help identify who should receive osteoporosis screening, including age and FRAX, OST, or SCORE tests.
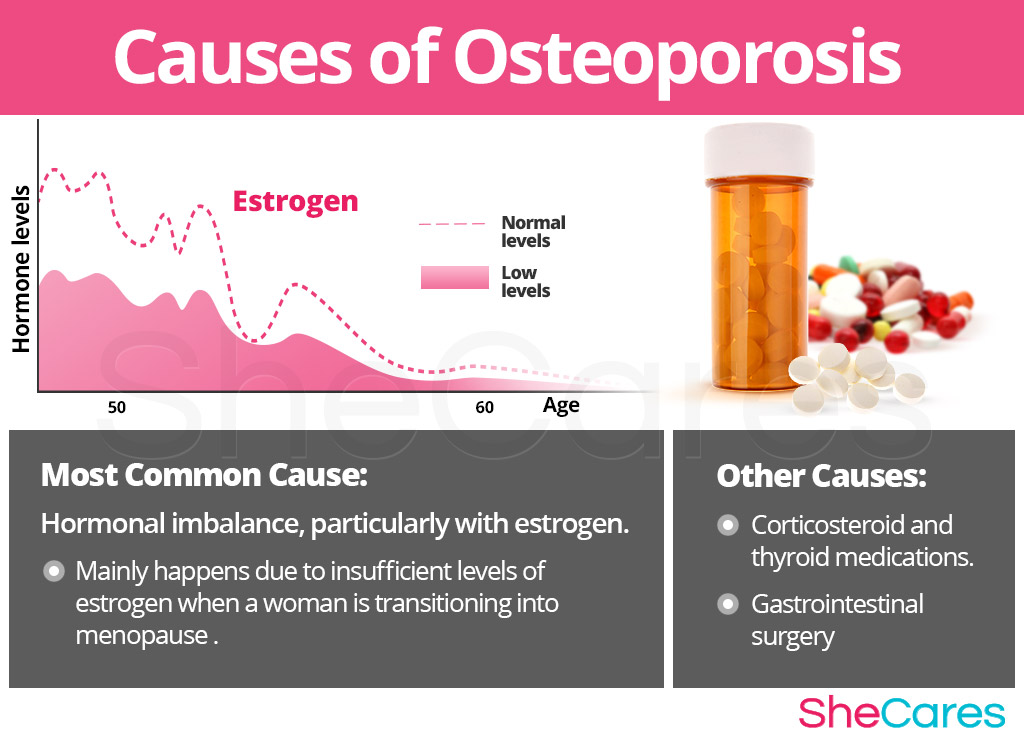
Causes
It is difficult to credit the cause of osteoporosis since the disease can be triggered by a variety of factors that differ from woman to woman. However, familiarizing oneself about the hormonal causes of osteoporosis provides a key to understanding how to help prevent this silent disease.
Hormonal Causes of Osteoporosis
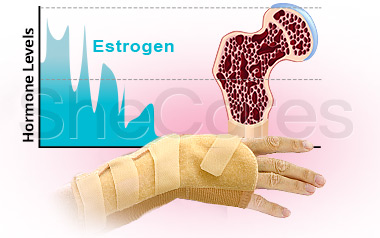
A female's reproductive life is characterized by the complex rise and fall of various reproductive hormones, such as estrogen and progesterone.
Estrogen is the female hormone that plays a key role in regulation of bone mass and strength by controlling activity of bone-resorbing osteoclasts and bone-forming osteoblasts.
Low estrogen levels can lead to weakened bones through pathological bone loss with fewer cells being produced. Low estrogen levels increase osteoclast formation and enhance bone resorption, a process by which the bone is broken down. Healthy estrogen levels inhibit osteoclasts' bone-resorbing activity. At the same time, an estrogen deficiency accelerates the death of osteoblasts, cells that deposit new bone tissue.
There are several stages within a woman's reproductive life in which it will be more likely for her to have osteoporosis, including pregnancy, breastfeeding, perimenopause, and postmenopause.
Other Less Common Causes of Osteoporosis
While hormonal imbalance is one of the major underlying causes of osteoporosis, experts also point out that osteoporosis may be caused by other, less common, underlying conditions, such as use of long-term medications, prior surgeries, genetic factors, and eating disorders.
Risk Factors and Triggers
Risk Factors for Osteoporosis
Risk factors for osteoporosis are characteristics that serve as potential reasons for women to have osteoporosis. Just because a woman may have several risk factors does not mean that she will automatically have osteoporosis with age. Once a woman is officially diagnosed, doctors will decipher the ultimate cause, determining if a risk factor for osteoporosis was to blame.
Some women are more likely than others to have osteoporosis because of health and behavioral risk factors. Health risk factors include age, family history, race and ethnicity, and various medical conditions, such as eating disorders, rheumatoid arthritis, or multiple sclerosis, among others. Behavioral risk factors include partaking in habits, such as smoking and drinking alcohol.

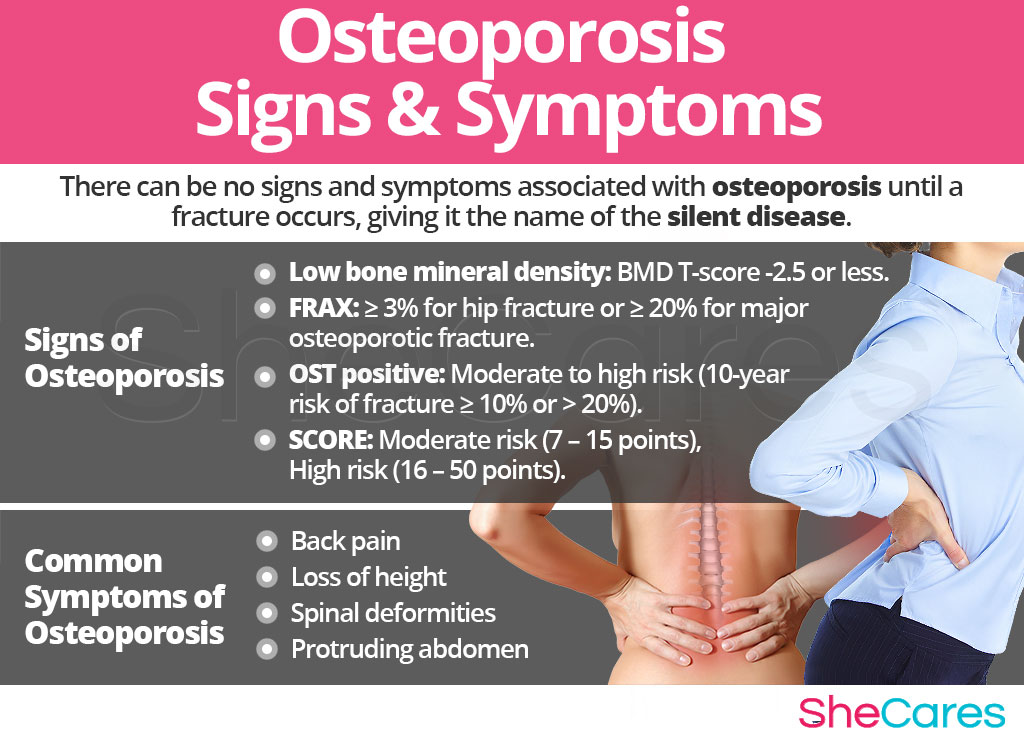
Signs and Symptoms
Because each woman's body is different, each one will experience possible progression of osteoporosis differently. However, keep in mind that often times, there are no signs and symptoms associated with osteoporosis until a fracture occurs, giving it the name of the silent disease.
Common Symptoms of Osteoporosis
- Back pain, caused by a fractured or collapsed vertebra
- Pain due to a bone fracture that occurred more easily than expected
- Loss of height
- Spinal deformities (such as stooped posture, sloping shoulders)
- Protruding abdomen
Signs of Osteoporosis
As opposed to more noticeable osteoporosis symptoms, medical signs are measurable criteria that are usually assessed by a physician. The following medical signs and scores from tests - such as FRAX, OST, and SCORE - will most likely be taken into account by a physician when diagnosing one's level of risk for obtaining osteoporosis with continued lifestyle choices.
- Bone fracture (hip, wrist, spine)
- Low bone mineral density: BMD T-score -2.5 or less
- FRAX: ≥ 3% for hip fracture or ≥ 20% for major osteoporotic fracture
- OST positive: Moderate to high risk (10-year risk of fracture ≥ 10% or > 20%)
- SCORE: Moderate risk (7 - 15 points), High risk (16 - 50 points)
Diagnosis of Osteoporosis
To diagnose and identify the symptoms of osteoporosis, a doctor must typically perform several procedures. First, he or she should review the patient's medical history, then conduct a physical exam, and finally do some testing. The doctor may order additional tests, if necessary.
Complications of Osteoporosis
When osteoporosis is undetected, it can lead to certain complications, which are more risky for a woman's physical health. However, it is important to remember that in the majority of cases, it is possible to prevent osteoporosis and take action so as not to require any serious medical intervention. In all matters, possible complications of osteoporosis can include bone fractures, limited mobility, and unexpected costs.
It is important to keep a watchful eye for any symptoms of osteopenia and monitor them properly in order to distinguish whether they're signaling the onset of osteoporosis. Women who have warning signs and/ or risk factors for osteoporosis may wish to manage or learn how to prevent further progression of the disease.
Prevention and Management
Preventing Osteoporosis
While preventing osteoporosis depends on the disease's cause and each person's predisposition, there are a few steps that a woman can take to halt its progression or lessen her chances of being osteoporotic later on in life.
It is important to note that after age 35, bone breakdown overtakes bone buildup, and this causes a gradual loss of bone mass.
That's why lifestyle adjustments to prevent osteoporosis from 30s and onwards are extremely crucial, especially with regard to diet, exercise, and healthy habits. Moreover, women may seek ways to complement these lifestyle approaches with alternative treatments for osteoporosis that help enhance the endocrine system and, therefore, help balance hormonal imbalances leading to onset of the disease.
Lifestyle Changes for Prevention
- Nutrition. Diet is key in preventing bone loss. By eating a balanced diet rich in fruits and vegetables that boost essential vitamin levels of calcium and vitamin D, it may be possible to ward off or prevent further progression of osteoporosis.
Regular exercise. Exercise on a regular basis to make bones and muscles stronger and prevent bone loss. The Centers for Disease Control and Prevention recommends that healthy adults get 150 minutes of exercise a week, which equates to 30 minutes daily most days of the week. Weight-bearing exercises for osteoporosis make muscles work against gravity and are best for preventing the disease. These activities include jogging, playing tennis, and lifting weights.
Healthy habits. It is important to limit alcohol consumption and quit smoking as it causes the body is produce less estrogen, the hormone that deters further progression of osteoporosis. Excessive alcohol also damages bones and can increase one's risk of falling and breaking a bone.
Supplements. In general, women need the following vitamins and minerals for optimal bone health: calcium, vitamin D, vitamin K, and magnesium. Supplements containing prescribed amounts of the nutrients needed to prevent osteoporosis should complement diet. Also, consider improving absorption of vitamin D by getting up to 10 minutes of sunscreen-free sun exposure up to three times daily, which also fosters calcium absorption. The time limit depends on skin type - and subsequent reaction to the sun - as well as the UV index.
Managing Osteoporosis
In whichever life stage a woman is in when diagnosed with osteoporosis, there are effective methods for osteoporosis management. Making minor daily changes and being conscientious can make a huge difference for women who are trying to handle osteoporosis.
Moreover, there are certain tips to follow that can help stop the progression of or worsen the disease, giving women the stepping stones they need to cope with the life stage. The following are general tips that women of all ages can use to control osteoporosis, such as partaking in safer exercise options and preventing falls.
While the aforementioned measures often help prevent osteoporosis and help manage the disease after its onset, they are unable to treat the root of the problem, which is hormonal imbalance. However, there are several natural treatments for osteoporosis that can help treat the hormonal causes.

Treatments
Osteoporosis treatments are based on one's estimated risk of breaking a bone within the next 10 years, which is taken from information such as the bone density test. With low risk, osteoporosis treatment may focus more on modifying risk factors and implementing lifestyle changes to prevent bone loss and falls instead of implementing medication.
Three Approaches to Treat Osteoporosis
Three levels of approaches can be considered for treating osteoporosis. These are categorized as: (1) Lifestyle Changes, (2) Alternative Medicine, and (3) Pharmaceutical Options.
If possible, women are encouraged to begin with the least risky approach for treating osteoporosis, which are lifestyle adjustments, and then proceed to the next level of care. Depending on the condition, medical intervention may be necessary to treat osteoporosis.
Lifestyle Changes for Osteoporosis
This primary level of treatment involves the least amount of risk; although, it conversely requires the highest amount of self-discipline. Often, simple changes in lifestyle can reap huge benefits in preventing further progression of bone loss and achieving a higher overall level of health. Fundamentally, an improved diet, regular exercise, and healthy habits can do a woman great service.
As previously mentioned with preventing osteoporosis, when considering nutrition, it is important to choose fruits and vegetables high in protein, calcium, and vitamin D to supplement the body while reducing caffeine and alcohol intake. Also, regular exercise should involve weight-bearing and strength-training exercises at least 30 minutes most days of the week to maintain bone mass.
Although these changes will help slow the progression of osteoporosis, they do not directly address hormonal imbalance, which is what leads to the disease's sudden onset. Further treatment may be necessary. Alternative medicine has proven to be an excellent way of treating osteoporosis related to the hormonal imbalance in a safe and natural way.
Alternative Medicine for Osteoporosis
Alternative medicines and supplements generally involve little to no risk and can be an effective way to avoid further progression of osteoporosis. In the case of herbal supplements, there are two main types to take into consideration: phytoestrogenic and hormone-regulating herbal supplements.
Phytoestrogenic herbal supplements
These supplements, such as red clover, contain estrogenic components produced by plants that help regulate hormones. By consuming certain plant-based estrogens, women can maintain higher estrogen levels to prevent or stop further progression of osteoporosis. Sufficient amounts of estrogen improves the building process of bones by inhibiting quicker degradation of bone mass.
Hormone-regulating herbal supplements
These supplements, including Macafem stimulate the endocrine system and treat the underlying hormonal imbalance. By promoting healthy estrogen levels, these supplements prevent or stop further progression of osteoporosis, such as osteoclastic activity with bone resorption and loss of bone density. They can be taken throughout a woman's life as they support the body's natural hormone production.
Additionally, there are some other types of supplements that can stop the progression of osteoporosis, including soy products.
A combination of approaches is usually the most effective route to take. Lifestyle changes combined with alternative medicine can ultimately prevent or slow down the progression of osteoporosis. However, for some women, the stage of osteoporosis they may be in may be so severe that more drastic treatment is necessary.
Pharmaceutical Options for Osteoporosis
Interventions at the third level involve the highest risk and often the highest costs. Not all treatments are suitable for women at every life stage; therefore, it is strongly recommended to speak to a licensed healthcare practitioner before starting any pharmaceutical osteoporosis treatment.
There are two main types of pharmaceutical options that can be prescribed to treat osteoporosis: bone-strengthening medication and hormone-regulating medication.
These three approaches are not mutually exclusive. A woman may use different approaches at different times or any combination of them, depending on the duration and severity of osteoporosis signs and symptoms. Today, more and more women find that dealing with osteoporosis can successfully be accomplished via a combination of healthy lifestyle and alternative treatments.

Sources
- Annals of the New York Academy of Sciences. (2009). Estrogens maintain bone mass by regulating expression of genes controlling function and life span in mature osteoclasts. Retrieved May 4, 2017, from https://www.ncbi.nlm.nih.gov/pubmed/19751412
- British Thyroid Foundation. (2015). Thyroid Disorders and Osteoporosis. Retrieved May 10, 2017, from http://www.btf-thyroid.org/information/leaflets/30-thyroid-disorders-and-osteoporosis-guide
- Cleveland Clinic. (n.d.). Menopause & Osteoporosis. Retrieved May 9, 2017, from https://my.clevelandclinic.org/health/articles/menopause-and-osteoporosis
- Cleveland Clinic. (n.d.). Menopause, Perimenopause, and Postmenopause. Retrieved May 9, 2017, from https://my.clevelandclinic.org/health/articles/what-is-perimenopause-menopause-postmenopause
- Harvard Health Publications. (2007). Depression among the risk factors for osteoporosis. Retrieved May 9, 2017, from http://www.health.harvard.edu/press_releases/depression-osteoporosis
- Journal of Bone and Mineral Research. (2014). Osteoporosis Screening in Postmenopausal Women 50-64 years-old: Comparison of U.S. Preventive Services Task Force Strategy and Two Traditional Strategies in the Women's Health Initiative. Retrieved May 9, 2017, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4117254/
- Journal of Natural Science, Biology and Medicine. (2011). Preventive effects of phytoestrogens against postmenopausal osteoporosis as compared to the available therapeutic choices: An overview. Retrieved May 4, 2017, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3276006/
- Mayo Clinic. (2016). Osteoporosis. Retrieved May 3, 2017, from http://www.mayoclinic.org/diseases-conditions/osteoporosis/home/ovc-20207808
- National Institutes of Health. (2015). Pregnancy, Breastfeeding, and Bone Health. Retrieved May 8, 2017, from https://www.niams.nih.gov/Health_Info/Bone/Bone_Health/Pregnancy/default.asp
- Northwestern University: Women's Health Research Institute. (n.d.). How Hormone Depletion Affects You. Retrieved May 9, 2017, from http://menopause.northwestern.edu/content/how-hormone-depletion-affects-you
- Physiology & Behavior. (2010). Estrogen regulation of apoptosis in osteoblasts. Retrieved May 4, 2017, from https://www.ncbi.nlm.nih.gov/pubmed/19426747
- State Government of Victoria, Australia: Department of Health & Human Services. (2016). Osteoporosis. Retrieved May 10, 2017, from https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/osteoporosis
- The American Congress of Obstetricians and Gynecologists. (2011). Osteoporosis. Retrieved May 9, 2017, from http://www.acog.org/Patients/FAQs/Osteoporosis
- The American Journal of Clinical Nutrition. (2001). Caffeine intake increases the rate of bone loss in elderly women and interacts with vitamin D receptor genotypes 1,2,3,4. Retrieved May 10, 2017, from http://ajcn.nutrition.org/content/74/5/694.full
- The Journal of Nutrition. (2006). Dietary Saturated Fat Intake Is Inversely Associated with Bone Density in Humans: Analysis of NHANES III. Retrieved May 10, 2017, from http://jn.nutrition.org/content/136/1/159.full
- U.S. Department of Health and Human Services: Office on Women's Health. (n.d.). Osteoporosis fact sheet. Retrieved May 8, 2017, from https://www.womenshealth.gov/publications/our-publications/fact-sheet/osteoporosis.html
- Vaananen HK & Harkonen PL. (1996). Estrogen and bone metabolism. Retrieved May 4, 2017, from https://www.ncbi.nlm.nih.gov/pubmed/8865143