What is PMDD?
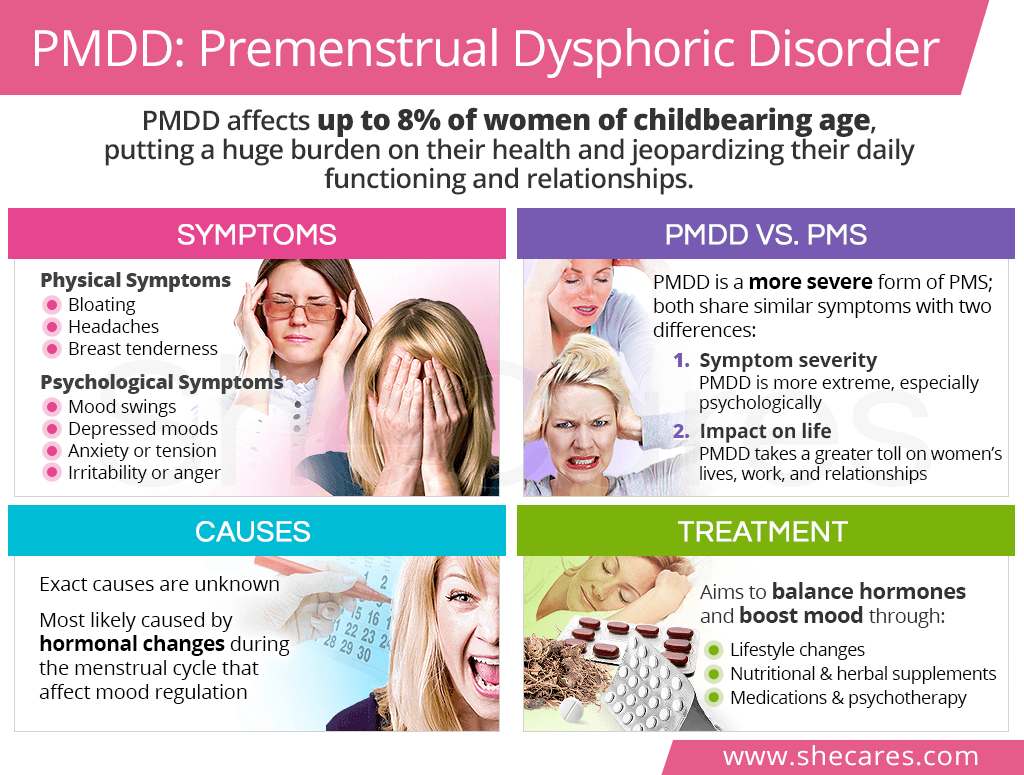
PMDD, or premenstrual dysphoric disorder, is classified as a menstrual disorder and considered a more severe form of premenstrual syndrome (PMS).
PMDD vs. PMS
For the most part, PMDD and PMS share the same symptoms. However, there are two important characteristics that differentiate the two, including:
The severity of experienced symptoms, with PMDD symptoms (particularly the psychological ones) manifesting in an extremer form
The impact the condition has on a woman's life, with PMDD taking a much greater toll on her functioning and relationships than PMS
PMDD Symptoms
Premenstrual dysphoric disorder symptoms, similarly to those of PMS, can begin as early as two weeks before a period. They affect women's physical and psychological well-being in the following ways:
Physical PMDD Symptoms
Psychological PMDD Symptoms
- Depressed mood
- Affective lability (e.g. mood swings, crying spells)
- Anxiety or tension
- Irritability or anger
- Loss of interest in daily activities
- Fatigue or low energy
- Difficulty concentrating
- A sense of being overwhelmed
- Significant appetite changes
- Sleep changes (insomnia or oversleeping)
PMDD Diagnosis
PMDD symptoms are often dismissed as a normal part of the menstrual cycle or wrongly diagnosed as mood disorders, like bipolar disorder.
However, to make the final PMDD diagnosis, the following criteria must be met:2,3,4
Symptoms must be cyclical, which means they only occur one or two weeks prior to the start of a period and disappear shortly after its onset; they are not present at other times during the menstrual cycle.
A woman reports at least five of the aforementioned PMDD symptoms, with at least one of them being:
- Affective lability
- Severe irritability or anger
- Feeling down or depressed
Severe anxiety or tension
- Symptoms disrupt family functioning, social roles, and work or school obligations.
PMDD Causes
Despite numerous medical advancements, the science is not clear on what causes PMDD.
It is thought that some women might be more sensitive to hormonal fluctuations during the menstrual cycle, which leads to a disruption of the production and release of mood-regulating chemicals, such as serotonin. This, in turn, affects their psychological well-being.
Additionally, it has been found that women who have a history of depression, anxiety, and bipolar disorder as well as those who have had significant mood changes postpartum are more prone to PMDD.5,6
PMDD Complications
PMDD complications mostly relate to the psychosocial distress the condition may cause. It can have the following negative consequences on women's daily functioning and life:
Reduced work or school productivity is experienced by 15% of women with intense menstrual symptoms, alongside a 14% absenteeism rate.7
Relationship conflicts - whether with one's partner, children, or friends – are a common struggle among women overwhelmed with PPMD symptoms.
Suicide is also a common complication, with up to 15% of women suffering from PMDD attempting to take their own life.2
PMDD Treatment

Premenstrual dysphoric disorder treatment can consist of natural methods to promote hormonal balance and boost mood, such as lifestyle changes and natural supplements, and conventional methods, including medications and psychotherapy.
Lifestyle Changes
Nutritious diet with foods rich in phytoestrogens and tryptophan-increasing proteins and complex carbohydrates may help reduce mood swings, irritability, and tension caused by PMDD.2
Regular exercises, like aerobics, can reduce period cramps and improve mood in women with PMS and PMDD.8
Stress-relief via body-mind techniques, like mindfulness or meditation, and a healthy sleep schedule can reduce cortisol levels and help women maintain a positive outlook on life.9
Addiction control, especially to alcohol and nicotine, is key to maintaining good physical and psychological health.
Alternative Medicine
Nutritional supplements, like calcium, omega-3 fatty acids, vitamin B6, or magnesium, may be a greatly beneficial PMDD treatment as they can reduce both physical and psychological symptoms of the condition.10,11,12,13
Phytoestrogenic supplements, like chasteberry or black cohosh, contain estrogenic compounds that can help balance hormones short-term and alleviate PMS and PMDD symptoms.
Hormone-regulating supplements, like Macafem, are one of the safest ways to achieve hormonal balance because they directly nourish the endocrine glands and help relieve symptoms long-term.
Conventional Medicine
PMDD medication most commonly consists of antidepressants, but it might also include birth control pills and pain relievers for physical discomforts.
Psychotherapy, such as cognitive therapy or psychoeducation, can be an effective treatment for PMMD and PMS, whether it is used alone or in combination with any of the aforementioned treatment options for improved results.
Key Takeaways
Perhaps because of its relatively low prevalence or similarities to PMS, premenstrual dysphoric disorder oftentimes does not receive the attention it needs. But the struggle women with PPMD endure is real and tremendous, cumulatively adding up to 3.8 years of their lives.14 This menstrual disorder brings about severe psychological symptoms, like mood swings or anger, alongside physical ones, like bloating or breast tenderness. While the exact cause of PMDD has not been discovered yet, it is most likely caused by hormonal changes during the menstrual cycle that affect mood regulation. Upon accurate diagnosis, women can find relief with various approaches, from lifestyle changes and herbal supplements – like Macafem Healthy Periods – to medications and psychotherapy. With a little effort and self-education, women can finally free themselves from monthly suffering once and for all!
Sources
- Harvard Review of Psychiatry. (2009). Update on Research and Treatment of Premenstrual Dysphoric Disorder. Retrieved February 25, 2020 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3098121/
- International Journal of Tryptophan Research. (2018). Analysis, Nutrition, and Health Benefits of Tryptophan. Retrieved February 25, 2020 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6158605/
- Journal of Ethnopharmacology. (2012). Black cohosh: coming full circle? Retrieved February 25, 2020 from https://www.ncbi.nlm.nih.gov/pubmed/22504147
- Journal of Psychiatry & Neuroscience. (2008). Premenstrual dysphoric disorder: burden of illness and treatment update. Retrieved February 25, 2020 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2440788/#r175-2
- Medline Plus. (2019). L-Tryptophan. Retrieved February 25, 2020 from https://medlineplus.gov/druginfo/natural/326.html
- Medline Plus. (2018). Premenstrual dysphoric disorder. Retrieved February 25, 2020 from https://medlineplus.gov/ency/article/007193.htm
- Office on Women's Health. (2018). Premenstrual dysphoric disorder (PMDD). Retrieved February 25, 2020 from https://www.womenshealth.gov/menstrual-cycle/premenstrual-syndrome/premenstrual-dysphoric-disorder-pmdd
- Pharmacological Reviews. (2016). Botanicals and Their Bioactive Phytochemicals for Women's Health. Retrieved February 25, 2020 from https://www.ncbi.nlm.nih.gov/pubmed/27677719
- Stat Pearls. (2019). Premenstrual dysphoric disorder. Retrieved February 25, 2020 from https://www.ncbi.nlm.nih.gov/books/NBK532307/
Footnotes:
- Casper. R. (2019). Patient education: Premenstrual syndrome (PMS) and premenstrual dysphoric disorder (PMDD). Retrieved February 25, 2020 from https://www.uptodate.com/contents/premenstrual-syndrome-pms-and-premenstrual-dysphoric-disorder-pmdd-beyond-the-basics
- Harvard Health Publishing. (2019). Treating premenstrual dysphoric disorder. Retrieved February 25, 2020 from https://www.health.harvard.edu/womens-health/treating-premenstrual-dysphoric-disorder
- Harvard Health Publishing. (2017). Premenstrual dysphoric disorder: It's biology, not a behavior choice. Retrieved February 25, 2020 from https://www.health.harvard.edu/blog/premenstrual-dysphoria-disorder-its-biology-not-a-behavior-choice-2017053011768
- Feingold. (2000). Diagnostic Criteria for Premenstrual Dysphoric Disorder (PMDD). Retrieved February 25, 2020 from https://www.ncbi.nlm.nih.gov/books/NBK279045/table/premenstrual-syndrom.table1diag/
- Mayo Clinic. (2018). Premenstrual dysphoric disorder: Different from PMS? Retrieved February 25, 2020 from https://www.mayoclinic.org/diseases-conditions/premenstrual-syndrome/expert-answers/pmdd/faq-20058315
- University of Iowa Hospitals & Clinics. (2018). Premenstrual dysphoric disorder (PMDD). Retrieved February 25, 2020 from https://uihc.org/health-topics/premenstrual-dysphoric-disorder-pmdd
- Journal of Occupational and Environmental Medicine. (2005). Estimating direct and indirect costs of premenstrual syndrome. Retrieved February 25, 2020 from https://www.ncbi.nlm.nih.gov/pubmed/15643156
- Women & Health Journal. (2015). The prevalence of self-reported premenstrual symptoms and evaluation of regular exercise with premenstrual symptoms among female employees in Taiwan. Retrieved February 25, 2020 from https://www.tandfonline.com/doi/abs/10.1080/03630242.2017.1296056
- American Journal of Obstetrics & Gynecology. (2003). An integrative medicine approach to premenstrual syndrome. Retrieved February 25, 2020 from https://www.ncbi.nlm.nih.gov/pubmed/12748452
- Reproductive Health. (2011). Essential fatty acids for premenstrual syndrome and their effect on prolactin and total cholesterol levels: a randomized, double blind, placebo-controlled study. Retrieved February 25, 2020 from https://www.ncbi.nlm.nih.gov/pubmed/21241460
- Taiwanese Journal of Obstetrics & Gynecology. (2009). Effects of calcium supplement therapy in women with premenstrual syndrome. Retrieved February 25, 2020 from https://www.ncbi.nlm.nih.gov/pubmed/19574172
- Office on Women's Health. (2018). Premenstrual Syndrome (PMS). Retrieved February 25, 2020 from https://www.womenshealth.gov/menstrual-cycle/premenstrual-syndrome
- National Institutes of Health. (2019). Vitamin B6. Retrieved February 25, 2020 from https://ods.od.nih.gov/factsheets/VitaminB6-Consumer/
- Psychoneuroendocrinology. (2003). The prevalence, impairment, impact, and burden of premenstrual dysphoric disorder (PMS/PMDD). Retrieved February 25, 2020 from https://www.ncbi.nlm.nih.gov/pubmed/12892987/