About Endometriosis
Endometriosis is a condition in which the lining of the uterus (called endometrium) grows outside of the uterus, most commonly in the ovaries and fallopian tubes. However, it can also develop in the vagina, cervix, bladder, bowel, and rectum.
In the first part of the menstrual cycle, endometrial growths feed on rising estrogen and may bleed and swell. This can lead to inflammation and scar tissue formation, triggering symptoms like pain, spotting between periods, and digestive problems.
Endometriosis is said to develop in over 11% of women.1 The condition is also a common underlying cause of infertility.
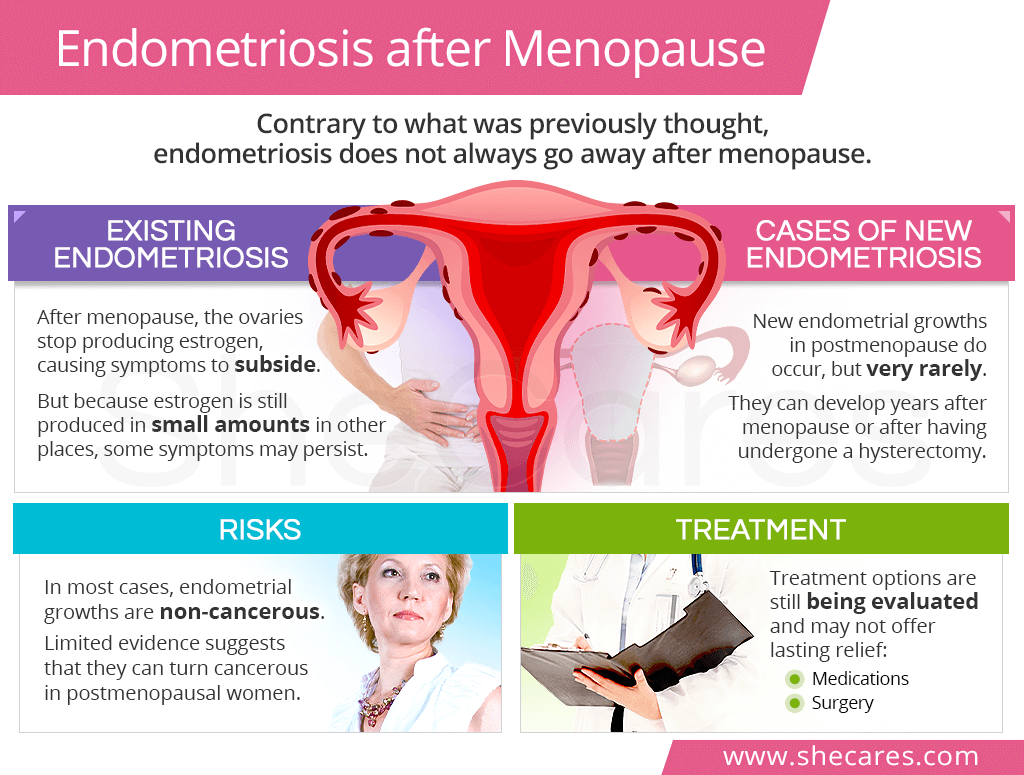
Endometriosis and Menopause
Endometriosis was previously considered a premenopausal condition, meaning that it only affected menstruating women. However, research shows that it can also develop after menopause in women with or without prior history of the condition.
What Happens to Endometriosis After Menopause?
Once women reach menopause, they stop menstruating. Their ovaries no longer produce estrogen, causing its levels to drop and continue low from then onwards.
As a result of this natural hormonal drop, the existing endometrial growths gradually shrink. As such, in the majority of women, symptoms of endometriosis after menopause subside.
However, estrogen continues to be produced in much smaller amounts in other body parts (e.g., adipose tissue). Despite estrogen lows, in some women, this may be enough for endometriosis symptoms to continue past menopause.
Cases of Endometriosis Developing After Menopause
Based on limited research data, a development of new endometrial growths after menopause is possible, yet very rare.2 In fact, it is said to affect 2-5% of postmenopausal women.3
It is unclear whether women with postmenopausal endometriosis had previously existent yet undiagnosed condition before reaching menopause that now produces clinical symptoms or if these growths developed after menopause without prior history of the condition.
Also, existing studies report cases of deep endometriosis in postmenopausal women (which is a more invasive stage that develops in organs such as bladder or ureters), rather than a superficial endometriosis common in premenopause.
Symptomatic endometrial growths can develop even years after menopause or having undergone a hysterectomy, a surgical removal of the uterus. They have also been seen in postmenopausal women taking hormone replacement therapy (HRT).
Risks of Endometriosis after Menopause
Endometriosis growths are typically benign, or non-cancerous. Besides painful symptoms and potential infertility that may negatively affect women's quality of life, they have not been associated with major health risks
However, there is limited evidence that, in rare cases, endometrial growths can turn cancerous, with a higher likelihood of it happening in postmenopausal women.3 Such malignant endometriosis commonly develops on the vagina.
Consequently, regular monitoring of the endometrial growths is highly important in postmenopausal women.
Postmenopausal Endometriosis Treatment
Postmenopausal endometriosis treatment will depend on whether a woman experiences symptoms.
If she reports no or mild symptoms, she can try to manage them naturally or with over-the-counter pain relievers, such as ibuprofen. Controlling postmenopausal weight gain and reducing obesity is also key since fat tissues produce estrogen that may feed the endometrial growths.
In the case a woman struggles with intense endometriosis symptoms, more advanced treatments may be necessary. They include the following:
Medications for endometriosis after menopause may include prescription pain relievers and a cautious use of aromatase inhibitors. Treatment with conjugated estrogen-bazedoxifene is also used in some cases to offer relief.
Surgery is generally the preferred treatment of endometriosis after menopause that causes symptoms. It can consist of removing the growths or scar tissue to relieve discomforts or it can consist of removing the uterus or ovaries.
Keep in mind that the effectiveness of various medications and surgical interventions for symptoms of endometriosis after menopause is still being studied. As such, they may not bring the desired results.
Key Takeaways
While endometriosis is predominantly a condition that affects menstruating women, new evidence shows that it can also touch women in postmenopause. Nevertheless, it is a rare and poorly understood phenomenon, potentially delaying the diagnosis process and causing women pain. Once they reach their last periods, consistency low estrogen levels usually cause symptoms of endometriosis after menopause to subside as endometrial growths feed on estrogen. However, in a small percentage of cases, symptoms persist or new growths develop years after women have been confirmed menopausal. Treatment options – such as medications or surgery – continue being investigated and may not offer lasting relief.
Sources
- Acta Obstetricia et Gynecologica. (2007). Postmenopausal endometriosis. Retrieved April 6, 2021 from https://obgyn.onlinelibrary.wiley.com/doi/pdf/10.1080/00016340701619407
- Current Opinion in Obstetrics and Gynecology. (2019). Postmenopausal endometriosis, where are we now? Retrieved April 6, 2021 from https://journals.lww.com/co-obgyn/Abstract/2019/08000/Postmenopausal_endometriosis,_where_are_we_now_.12.aspx
- Gynecological Surgery. (2019). Symptomatic endometriosis developing several years after menopause in the absence of increased circulating estrogen concentrations: a systematic review and seven case reports. Retrieved April 6, 2021 from https://gynecolsurg.springeropen.com/articles/10.1186/s10397-019-1056-x
- Harvard Health Publishing. (2021). Endometriosis. Retrieved April 6, 2021 from https://www.health.harvard.edu/diseases-and-conditions/endometriosis2
- Harvard Health Publishing. (2019). Will my endometriosis go away after menopause? Retrieved April 6, 2021 from https://www.health.harvard.edu/womens-health/will-my-endometriosis-go-away-after-menopause
- Human Reproduction Update. (2017). The management of menopause in women with a history of endometriosis: a systematic review. Retrieved April 6, 2021 from https://academic.oup.com/humupd/article/23/4/481/3814217
- Journal of Medical Case Reports. (2009). Endometriosis in a postmenopausal woman without previous therapy: a case report. Retrieved April 6, 2021 from https://jmedicalcasereports.biomedcentral.com/articles/10.1186/1752-1947-3-135
- Journal of Mid-Life Health. (2014). Postmenopausal endometriosis: An enigma revisited. Retrieved April 6, 2021 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4264277/
- Office on Women's Health (2019). Endometriosis. Retrieved April 6, 2021 from https://www.womenshealth.gov/a-z-topics/endometriosis
- Women's Health. (2015). Endometriosis after menopause. Retrieved April 6, 2021 from https://journals.sagepub.com/doi/pdf/10.2217/whe.15.59
Footnotes:
- Fertility & Sterility. (2011). Incidence of endometriosis by study population and diagnostic method: the ENDO study. Retrieved April 6, 2021 from https://pubmed.ncbi.nlm.nih.gov/21719000/
- Case Reports in Gastrointestinal Medicine. (2018). Postmenopausal Deep Infiltrating Endometriosis of the Colon: Rare Location and Novel Medical Therapy. Retrieved April 6, 2021 from https://www.hindawi.com/journals/crigm/2018/9587536/
- Diagnostics. (2020). Endometriosis in Menopause - Renewed Attention on a Controversial Disease. Retrieved April 6, 2021 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7151055/
- Journal of Clinical Pathology. (2008). A detailed morphologic and immunohistochemical comparison of pre- and postmenopausal endometriosis. Retrieved April 6, 2021 from https://pubmed.ncbi.nlm.nih.gov/17908802/