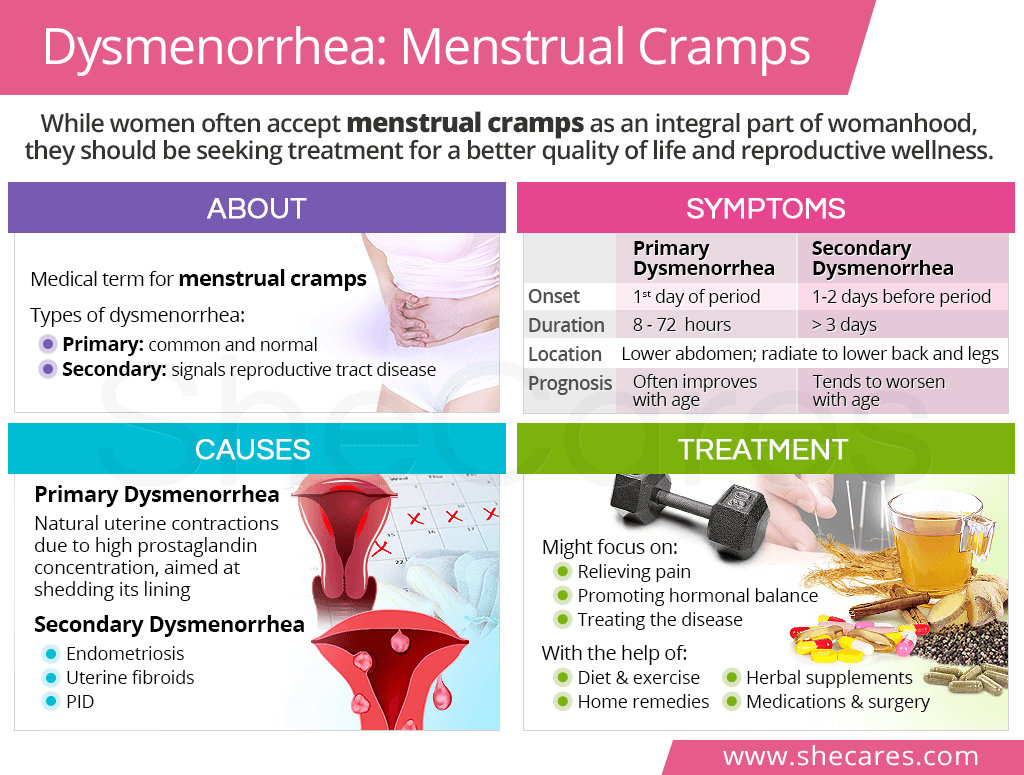
What is Dysmenorrhea?
Dysmenorrhea is a medical term for painful menstrual cramps. It is the most common menstrual disorder and source of pelvic pain, both acute and chronic, in women of reproductive age.2
Types of Dysmenorrhea
Dysmenorrhea can be classified into two types:
Primary dysmenorrhea: common menstrual cramps without abnormal causes
Secondary dysmenorrhea: period pain that signals a reproductive tract disorder
It is important to note that dysmenorrhea is not the same as premenstrual syndrome (PMS), although menstrual cramps can be one of the symptoms of PMS.
Dysmenorrhea Symptoms
Dysmenorrhea symptoms, especially their duration, may vary slightly depending on whether it is due to primary or secondary causes. They are as follows:3,4
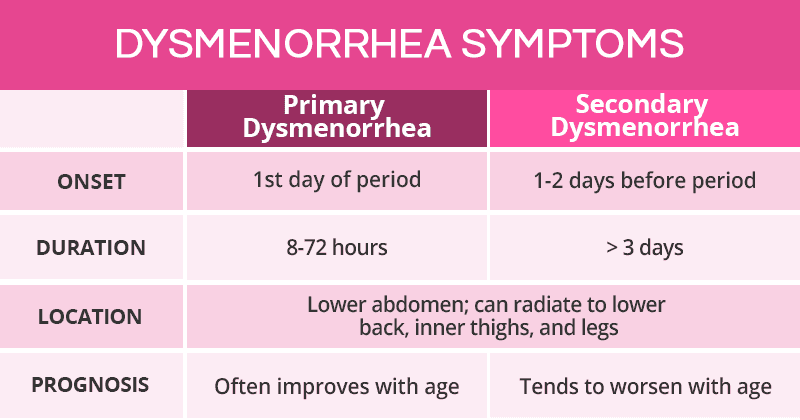
Other symptoms of primary dysmenorrhea may include nausea, headache, or diarrhea, all of which usually improve over the years and after childbirth. On the other hand, secondary dysmenorrhea, depending on the cause, can include specific symptoms that tends to worsen with age, such as intermenstrual bleeding, menorrhagia, and infertility,
Dysmenorrhea Causes
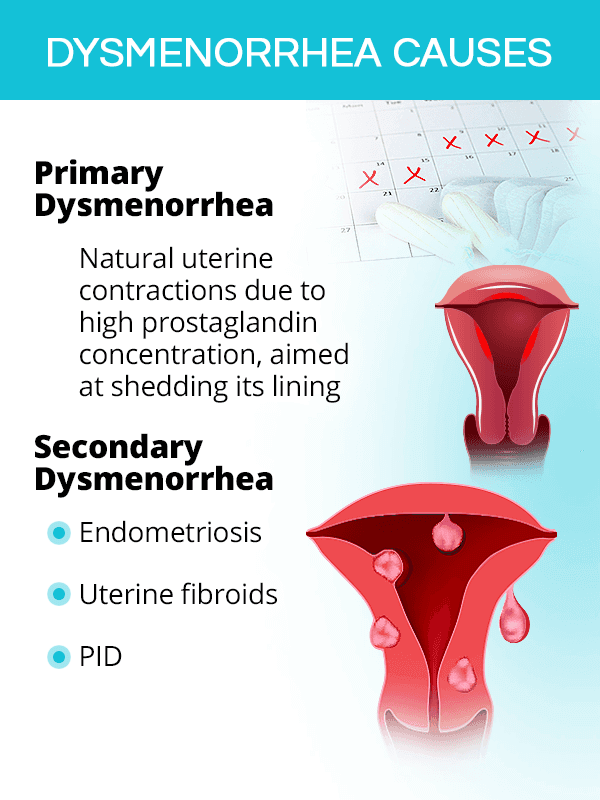
Menstrual cramps are mainly rooted in hormonal imbalance.
They can either have natural causes related to the physiological changes occurring during a period (primary dysmenorrhea) or abnormal causes related to a disease of the reproductive organs (secondary dysmenorrhea).
Primary Dysmenorrhea Causes
Primary dysmenorrhea is caused by natural uterine contractions, which occur to help the uterus shed its lining.
In fact, a period is simply that: the shedding of the endometrial lining that has thickened in the first part of the menstrual cycle in preparation for potential pregnancy. When pregnancy does not occur, this lining is shed with the help of uterine contractions, which are triggered by natural chemicals called prostaglandins.
For unknown reasons, some women have higher concentrations of prostaglandins, which produces stronger uterine contractions, thus constricting the blood vessels in the uterus and resulting in menstrual pain.
Secondary Dysmenorrhea Causes
Secondary dysmenorrhea is caused by a disease of the reproductive tract, which might include any of the following:
- Endometriosis
- Adenomyosis
- Uterine fibroids
- Pelvic inflammatory disease (PID)
- Endometrial polyps
- Cervical stenosis
Complications of Dysmenorrhea
Unresolved menstrual cramps, especially when severe, can have detrimental effects on numerous aspects of a woman's life, including the following:
Quality of Life. Up to 33% of women report such severe period cramps that they disable them from participating in daily activities, getting enough sleep, maintaining social bonds, and enjoying life for a few days each month.5
Work or School Performance. For teenagers and adolescents, dysmenorrhea is the leading cause of missing school or work.6
Mental Health. Being stricken with intense period pains on a regular basis has also been found to have detrimental effects on young women's mental health, including causing depression and anxiety.7
Overall Health. Since secondary dysmenorrhea occurs due to an underlying condition, not finding adequate treatment can lead to its progression, thus causing further damage to a woman's reproductive health and taking a bigger toll on her life.
Dysmenorrhea Treatment
A key factor in choosing the right treatment for menstrual cramps is whether it has normal or abnormal causes.
Generally, women are advised to promote hormonal balance through lifestyle changes and alternative medicine, before moving to conventional medicine.
Lifestyle Changes for Period Pain
Nutritious diet with complex carbohydrates, protein, and healthy fats is key to optimal menstruation health, including regular and pain-free periods. Adding phytoestrogenic foods, like flax or oats, is also beneficial.
Regular exercise has shown significant improvements in lowering period pains, most probably due to their effects of stimulating blood flow to the pelvis and the release of pain-relieving endorphins.8
Home remedies, like applying a heating pad or hot water bottle, are some of the most popular and effective dysmenorrhea treatment approaches, especially for mild to moderate discomforts.
Alternative therapies, like acupuncture or massage, can help with menstrual cramps through a variety of actions, although scientific research on their effectiveness is still scarce.
Alternative Medicine for Period Pain
Nutritional supplements, like fish oil, thiamine, pyridoxine, and magnesium, have been shown to aid in reducing the severity or duration of menstrual cramps.3
Phytoestrogenic supplements, like ginseng, contain plant-based compounds that mimic the action of estrogen in the body, thus contributing to balancing hormones and relieving painful periods.
Hormone-regulating supplements, like Macafem, can be effective in relieving menstrual pain by nourishing the endocrine glands to regulate hormone production and menstrual cycles.
Conventional Medicine for Period Pain
Medications are mainly oriented towards relieving period pain and inhibiting prostaglandins with analgesics or birth control pills. Secondary dysmenorrhea treatment will focus on managing the underlying cause.
Surgery can be necessary for severe menstrual cramps due to uterine fibroids or endometriosis, whether it consists of their removal, growth inhibition, or - in rare cases - uterus removal, known as a hysterectomy.
Key Takeaways
Women often accept menstrual cramps as an integral part of womanhood, not knowing that experiencing intense period pain can and should be treated. While most discomforts during menses are caused by normal uterine contractions that help shed the lining (primary dysmenorrhea), some have symptoms that are indicative of a disease of the reproductive tract, thus calling for proper evaluation (secondary dysmenorrhea). Treatment will depend on the exact cause of period cramps, ranging from lifestyle changes of a healthy diet, exercise, and natural remedies to herbal supplements, like Macafem Healthy Periods for optimal menstrual health, to medications aimed at relieving the pain and treating the underlying conditions that cause it. With the right initiative, women can reduce or eliminate period pain for a better quality of life for years to come!
Sources
- Better Health Channel. (2018). Menstruation - pain (dysmenorrhea). Retrieved February 11, 2020 from https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/menstruation-pain-dysmenorrhoea
- Medline Plus. (2018). Painful menstrual periods. Retrieved February 11, 2020 from https://medlineplus.gov/ency/article/003150.htm
- Medline Plus. (2019). Period Pain. Retrieved February 11, 2020 from https://medlineplus.gov/periodpain.html
Footnotes:
- American Family Physician. (2014). Diagnosis and Initial Management of Dysmenorrhea. Retrieved February 11, 2020 from https://www.aafp.org/afp/2014/0301/p341.html
- American College of Obstetricians and Gynecologists. (2015). Dysmenorrhea: Painful Periods. Retrieved February 11, 2020 from https://www.acog.org/Patients/FAQs/Dysmenorrhea-Painful-Periods
- Cleveland Clinic. (2014). Dysmenorrhea. Retrieved February 11, 2020 from https://my.clevelandclinic.org/health/diseases/4148-dysmenorrhea
- The BMJ. (2006). Diagnosis and management of dysmenorrhoea. Retrieved February 11, 2020 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1459624/
- F1000 Research. (2017). Dysmenorrhea and related disorders. Retrieved February 11, 2020 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5585876/
- American Family Physician. (2005). Dysmenorrhea. Retrieved February 11, 2020 from https://www.aafp.org/afp/2005/0115/p285.html
- The Journal of Adolescent Health. (2009). Menstrual symptoms in adolescent girls: association with smoking, depressive symptoms, and anxiety. Retrieved February 11, 2020 from https://www.ncbi.nlm.nih.gov/pubmed/19237109/
- Journal of Education and Health Promotion. (2018). The Effect of aerobic exercise on primary dysmenorrhea: A Clinical trial study. Retrieved February 11, 2020 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5791467/