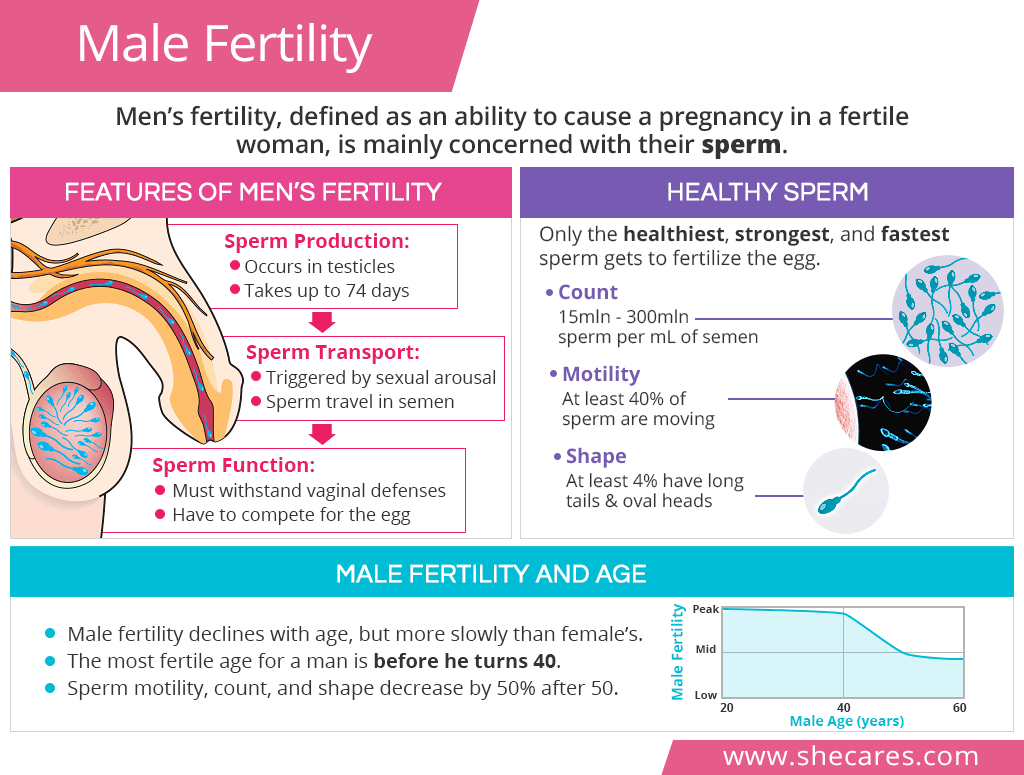
Features of Men’s Fertility
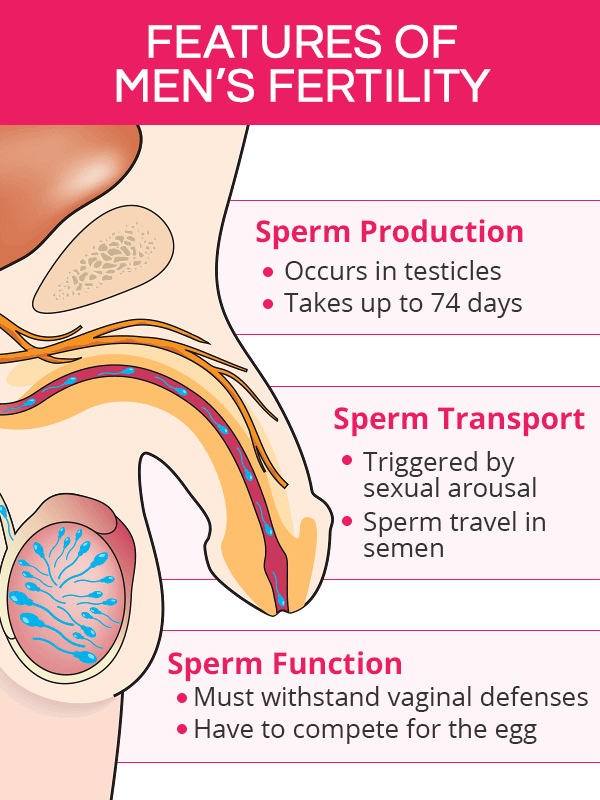
Male fertility is all about the sperm. For the sperm to be able to fertilize the eggs during ovulation, their production, transport, and function have to be maximally optimized and synchronized.
Sperm Production
It takes about 72-74 days from the moment the sperm are produced and until they are mature enough to be used for their designated functions.
Sperm production is governed by the hormone testosterone. When the hypothalamus detects low testosterone levels, it triggers a cascade of hormonal changes to produce more testosterone in order to make more sperm.
Sperm are made within the testicles. When they mature, grow a tail, and learn to swim, the sperm are stored within the testes for up to three weeks until potential ejaculation. If ejaculation does not occur, the body recycles them.
Because sperm are sensitive to temperature changes, testicles and the scrotum that contains them are maintained at temperatures up to three degrees Celsius lower (5.4°F) than the rest of the body.
Any abnormalities during the production or maturation process, such as hormonal imbalance or overheating, can affect sperm's health and often make it unviable for conception, thus compromising a male's fertility.
Sperm Transport
Sperm's transport from the testes and out of the body is triggered by sexual arousal.
Sperm travels in semen, also called seminal fluid, whose function is to ease sperm motility through the female reproductive tract, protect them from possible damage, and provide key nutrition to ensure their survival in a woman's body for up to 5 days.
Once ejaculation is near, the sperm mixes with the seminal fluid and is pushed out of the body through the penis' urethra. An average ejaculate contains up to 300 million sperm. After ejaculation, it takes about one or two days for semen to be replenished.
Besides nutrients, the viruses and bacteria causing sexually transmitted diseases (STDs) are also carried with semen.
Male fertility can be diminished when there is a disturbance in any part of sperm transport, including mixing with semen; blockages within the testicles, ejaculatory ducts, or urethra; or ejaculation itself.
Sperm Function
Once inside a woman's reproductive tract, sperm have numerous challenging tasks to complete. Only the healthiest, strongest, and fastest sperm get to fertilize the egg.
Female cervical fluid is very selective and does not let abnormal or slow sperm pass from the vagina through the cervix. As a result, only a small fraction of them, about 100,000, pass through the cervix, and less than 200 make it to the end of the fallopian tubes.
The contractions of the female's uterus help move the sperm further up to meet the egg, a journey of about 6 inches (15 cm) that takes from 30-60 minutes for fast-swimming sperm to several days for slower swimmers.
Once near the egg, the sperm have to penetrate through the egg's three protective layers, which takes about 24 hours. As soon as the first sperm is inside, the eggs sends a signal that it is fertilized, blocking all subsequently entering sperm.
Healthy Sperm
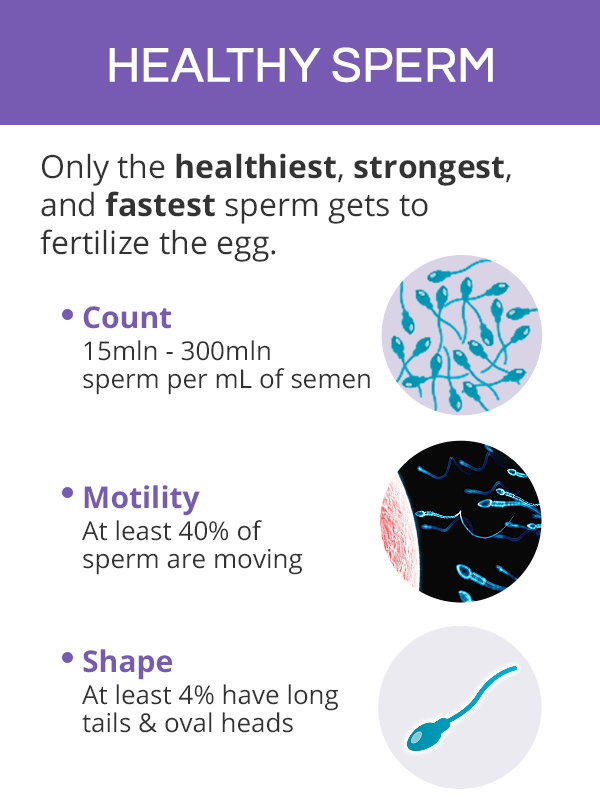
As discussed above, sperm have to be strong and healthy to get through the natural defenses of the selective reproductive tract and compete for the egg against other sperm.
Sperm's health, which determines men's fertility, has the following main characteristics:
Count. A healthy ejaculate (a discharge in one, single ejaculation) contains between 15 million to 300 million sperm per milliliter (mL) of semen. An average semen volume is about 2 mL, although values ranging from 1.5 mL to 6.8 mL are considered normal.
Movement (or motility). Normal sperm motility is when at least 40% of sperm are moving, with a minimum of 32% “moving progressively,” which means they are moving in either a straight line or large circles. Poor sperm motility is a common cause of reduced male fertility.
Shape (or morphology). Healthy sperm have long tails and oval heads that are covered in caps, called acrosomes. Abnormal sperm can have two heads, be missing tails, and more. Most commonly accepted criteria require at least 4% to be without abnormalities to be considered healthy.
When semen is analyzed in the laboratory, there are other features being evaluated besides the three aforementioned to evaluate male fertility, including sperm viability or pH.
Male Fertility and Age
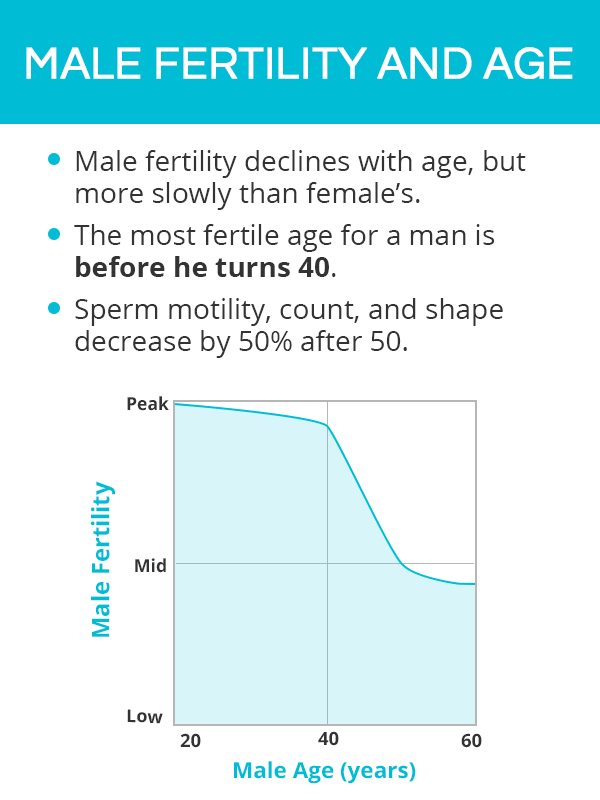
Even though the decline of male fertility over time is not as drastic as in the case of female fertility, studies have shown that age does contribute to a reduction in pregnancies and an increased time in achieving pregnancy.
Although a man's testicles produce sperm throughout his life, their health characteristics do not remain the same across the years. Studies have found the following changes in men's fertility due to age:
Sperm motility, count, and shape peak before the age of 25 and decrease by over 50% by the age of 55.
Semen quality is at its best between the ages of 30 and 35 and reaches its lowest levels after 55.
It might take men older than 45 up to five times longer to conceive than those 25 and younger.
Success rates of in vitro fertilization (IVF) are five times lower if the man is over 40.
The risks of miscarriage, autism, and genetic mutations are also much higher in men after 40.
This data shows that the most fertile age for a man is before he turns 40, and - although it is very much possible for an older man to father a child - it might take longer to cause a pregnancy in his fertile partner.
Besides age, male fertility can also be negatively affected by prolonged stress, smoking, poor diet, STDs, and obesity, among others. Read more about male infertility.
Key Takeaways
Men's fertility revolves around their sperm. These microscopic cells face numerous challenges on their way to complete their life mission, fertilize the egg. Because only the healthiest, fastest¸ and strongest sperm wins the race for the egg, ensuring ideal sperm health by optimizing their production, transport, and function is of great essence. Certain factors, such as age, have to be taken into consideration when evaluating male fertility as studies have shown that their ability to father children decrease past the age of 40. Nevertheless, pregnancy with older men is still very feasible, though it make longer to achieve it.
Sources
- American Society for Reproductive Medicine. (2018). Sperm Morphology (Shape): Does It Affect Fertility? Retrieved November 21, 2018 from https://www.reproductivefacts.org/news-and-publications/patient-fact-sheets-and-booklets/documents/fact-sheets-and-info-booklets/sperm-morphology-shape-does-it-affect-fertility/
- American Pregnancy Association. (2018). Male Fertility Testing. Retrieved November 21, 2018 from http://americanpregnancy.org/infertility/male-fertility-testing/
- Cleveland Clinic. (n.d.). Genetic Testing and male Factor Infertility. Retrieved November 21, 2018 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4594528/
- Communicative and Integrative Biology. (2015). Why so many sperm cells? Retrieved November 21, 2018 from
- Human Reproduction Update. (2006). Sperm transport in the female reproductive tract. Retrieved November 21, 2018 from https://academic.oup.com/humupd/article/12/1/23/607817
- Mayo Clinic. (2018). Healthy sperm: Improving your fertility. Retrieved November 21, 2018 from https://www.mayoclinic.org/healthy-lifestyle/getting-pregnant/in-depth/fertility/art-20047584
- Mayo Clinic. (2018). Male infertility. Retrieved November 21, 2018 from https://www.mayoclinic.org/diseases-conditions/male-infertility/symptoms-causes/syc-20374773
- Methods in Molecular Biology. (2014). Genetics of male fertility. Retrieved November 21, 2018 from https://www.ncbi.nlm.nih.gov/pubmed/24782004
- National Healthy System. (2016). Low sperm count. Retrieved November 21, 2018 from https://www.nhs.uk/conditions/low-sperm-count/
- Rengan, Anil at al. (2015). Unexplained Infertility: Pathophysiology, Evaluation and Treatment. New York, NY: Springer.