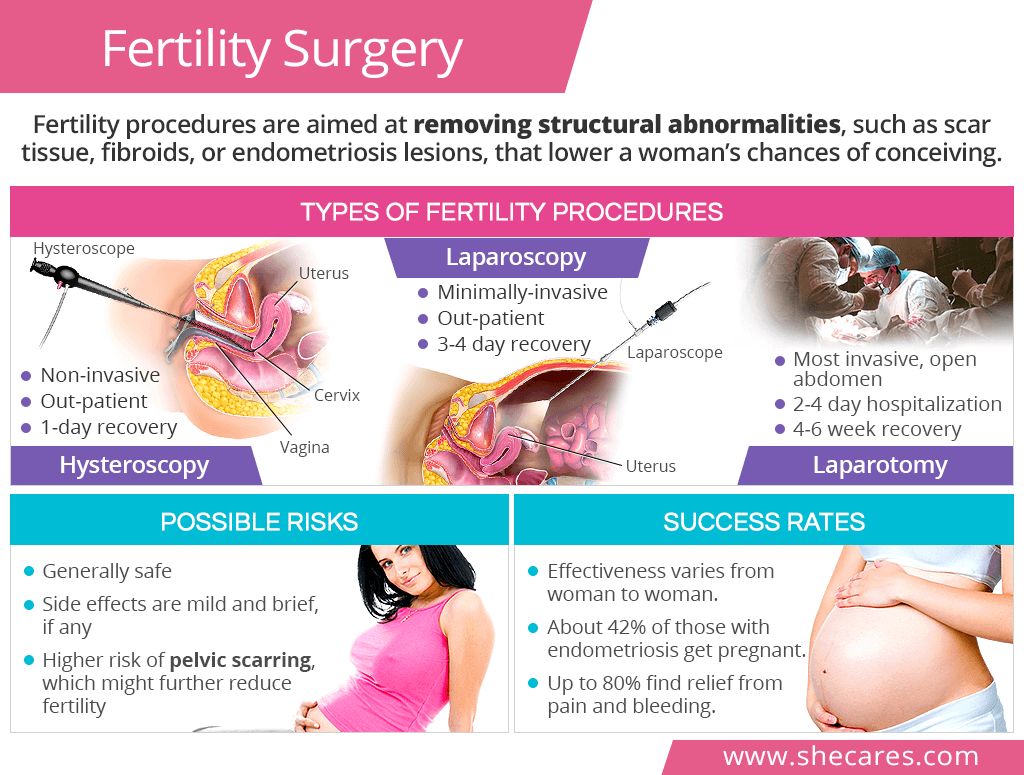
Types of Fertility Procedures
Fertility procedures can be both diagnostic and operational. It means that they allow the surgeon to look into the reproductive organs to locate the cause of fertility problems as well as appropriately remove it.
Surgical options for treating infertility - listed from the least to the most invasive - are as follows:
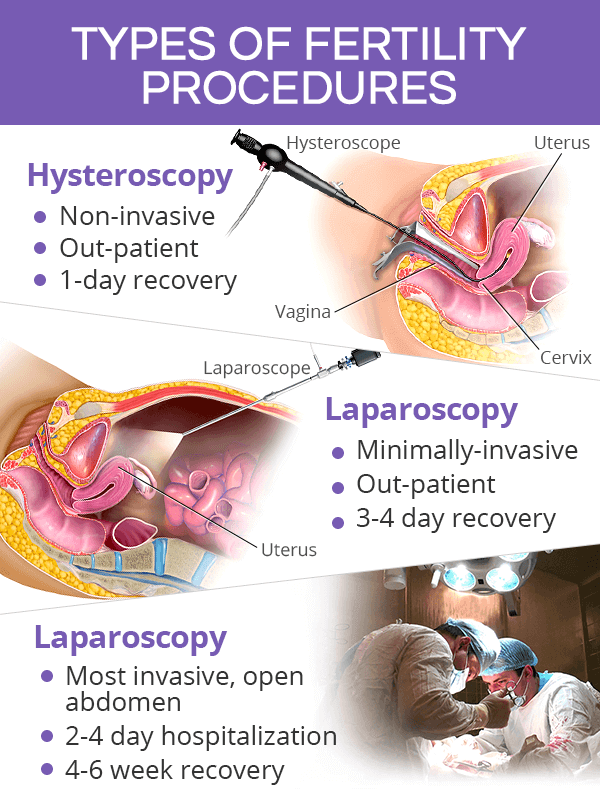
Hysteroscopy for Infertility
Hysteroscopy is a non-invasive procedure, during which a device called a hysteroscope is inserted through the vagina, past the cervix, and into the uterus. There are no incisions made in the abdomen or pelvis during hysteroscopy, and it is performed as an outpatient procedure.
Hysteroscopic fertility surgery can be helpful in treating problems within the uterus, such as uterine polyps or fibroids, abnormal bleeding, and other problems responsible for recurrent miscarriages.
Laparoscopy for Infertility
Laparoscopy, also known as keyhole surgery, is a minimally invasive fertility surgery, which consists of making small incisions in the abdomen and inserting a device called a laparoscope into the body cavity. This outpatient procedure is performed under general anesthesia.
It allows a surgeon to examine the abdomen and pelvis with all reproductive organs in order to remove ovarian cysts, fibroids, fallopian tube blockage, endometriosis lesions, and scar tissue. It can also be used in women with polycystic ovarian syndrome (PCOS) to induce ovulation through ovarian drilling, among other techniques. Some infertility clinics perform robotic laparoscopic surgeries, which enables them to do reproductive repairs that would normally require an open surgery.
Laparotomy for Infertility
Laparotomy is the most invasive fertility surgery, which is performed on an open abdomen with an incision that resembles one made for a cesarean section.
Usually the last resort, laparotomy is done when the size, location, or number of uterine fibroids does not allow for their removal through less invasive procedures. It can also be effective in tubal ligation reversal or advanced causes of endometriosis.
Fertility Surgery Risks

Fertility procedures are generally safe, and the risk of serious complications is low.
Possible Side Effects
General and usually mild side effects of fertility surgery include nausea and dizziness from anesthesia; irritation at the incision site; or bladder infections. Although very rare, more serious side effects might consist of bleeding; infections; a perforation of the reproductive organs; or formation of internal adhesions, among others.
Severe abdominal pain, vomiting, fever, pus from the incision site, or bleeding might signal serious complications and should be brought to the immediate attention of a doctor.
Pelvic Scarring
Surgical interventions for fertility increase the risk of the formation of scars or adhesions within the pelvis, which might further diminish a woman's chances of conception. The highest rates of scarring are seen is laparotomies in comparison to the other two fertility surgeries.
Post-Operative Recovery
Hysteroscopy for infertility does not require hospitalization, and women can resume their activities the next day.
Laparoscopy for infertility allows women to go home the same day and return to their activities within 3 to 4 days.
Laparotomy requires a hospital stay for a few days, and women can resume their activities in 4 to 6 weeks.
Fertility Surgery Success Rates
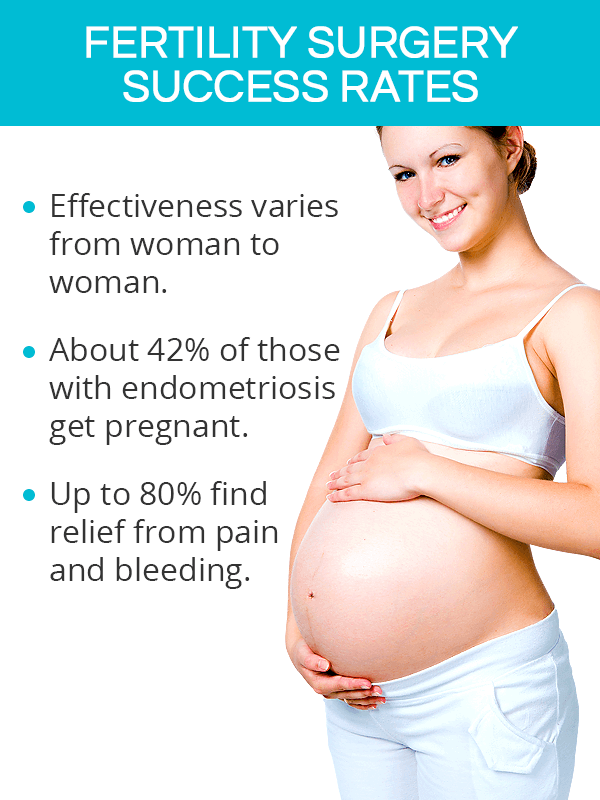
Success rates for infertility surgery are difficult to obtain. Whether a woman achieves pregnancy after undergoing surgery depends on what was the underlying cause and whether there was permanent damage to reproductive organs. Women's age, overall health, and reproductive history also play important roles.
Most available statistical data on efficacy of fertility surgery relates to fertility problems rooted in endometriosis:
The pregnancy rate for women with endometriosis who have had a laparoscopic fertility surgery is almost 42%.
A reduction of pain and bleeding due to endometriosis with laparoscopy has been found successful in up to 80% of women.
Women with advanced endometriosis benefit from fertility procedures more than those with milder forms.
In the case of damaged fallopian tubes, it might be impossible to do repairs and restore their function with fertility surgery. As such, women are advised to consider taking advantage of assisted reproductive technologies (ARTs), such as in vitro fertilization (IVF).
Key Takeaways
For women whose struggles with infertility are caused by structural abnormalities within the reproductive tract, fertility surgery is often the last option to restore their chances of conceiving. There are three types of fertility procedures: hysteroscopy, a non-invasive surgery that allows for removal of polyps and fibroids within the uterus; laparoscopy, a minimally-invasive procedure useful in removing ovarian cysts, tubal blockage, and endometriosis lesions; and laparotomy, an invasive procedure performed on an open abdomen to remove large fibroids or other advanced fertility issues. Infertility procedures are generally safe, but whether they restore a woman's fertility and lead to a healthy conception depends on numerous factors, including the cause of infertility, extent of organ damage, and a woman's age, among others.
Sources
- American College of Obstetricians and Gynecologists. (2017). Treating Infertility. Retrieved December 10, 2018 from https://www.acog.org/Patients/FAQs/Treating-Infertility
- American Society for Reproductive Medicine. (2016). Laparoscopy and Hysteroscopy. Retrieved December 10, 2018 from https://www.reproductivefacts.org/globalassets/rf/news-and-publications/bookletsfact-sheets/english-fact-sheets-and-info-booklets/booklet_laparoscopy_and_hysteroscopy.pdf
- Cleveland Clinic. (2018). Hysteroscopy. Retrieved December 10, 2018 from https://my.clevelandclinic.org/health/treatments/10142-hysteroscopy
- Clinical and experimental reproductive Medicine. (2013). Natural conception rate following laparoscopic surgery in infertile women with endometriosis. Retrieved December 10, 2018 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3630290/
- Eunice Kennedy Shriver National Institute of Child Health and Human Development. (2017). Infertility Treatments for Females. Retrieved December 10, 2018 from https://www.nichd.nih.gov/health/topics/infertility/conditioninfo/treatments/treatments-women
- Washington University Physicians. (n.d.). Fertility Surgery: Women. Retrieved December 10, 2018 from https://fertility.wustl.edu/treatments-services/infertility-surgery/