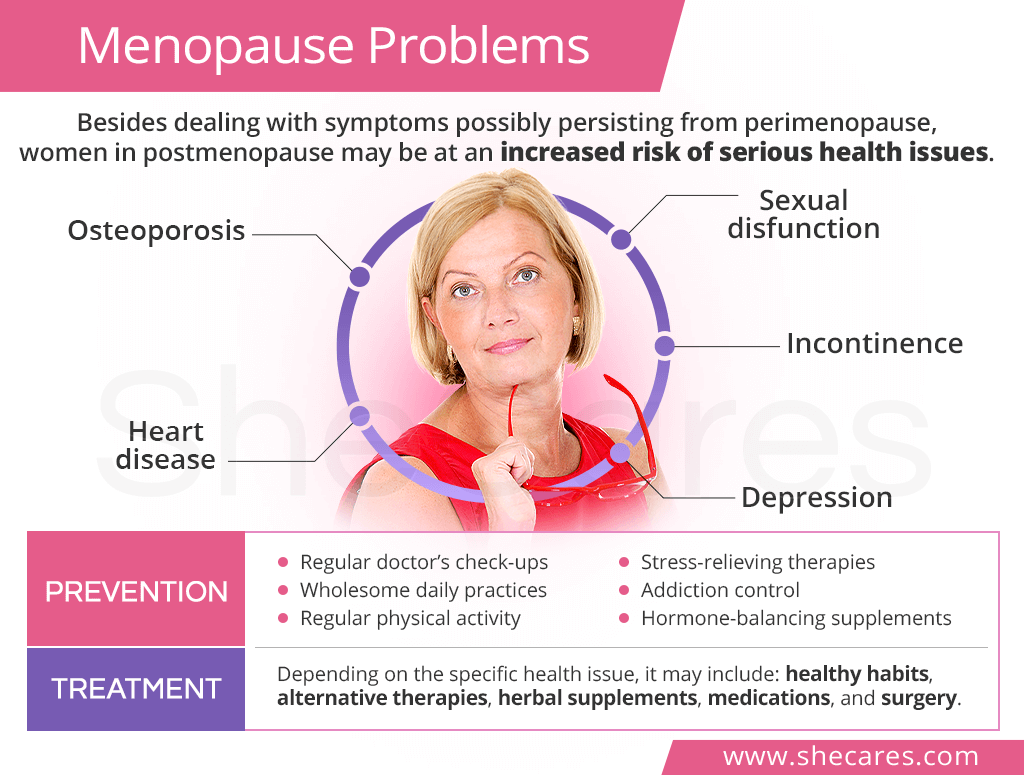
Osteoporosis
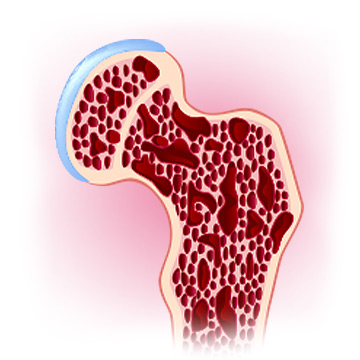
Osteoporosis is one of the main menopause problems of which women should be mindful. It is characterized by low bone density and bone fragility, which manifest 10 to 15 years after menopause.1
Estrogen plays a key role in maintaining bone health by regulating the activity of osteoclasts and osteoblasts, which are bone-forming and bone-resorbing cells. After menopause, estrogen levels go down, causing bone density loss since there is more bone being resorbed than formed. As a result, women are at a higher risk of fractures.
What Can Be Done?
Prevention of osteoporosis after menopause consists of eating a healthy diet, ensuring adequate intake of calcium and vitamin D, staying physically active to maintain mobility and a healthy weight, and quitting smoking.
In addition, postmenopausal women over the age of 65 are recommended to undergo a bone mineral density scan; women under 65 with known risk factors should undergo it sooner.2
Heart Disease
Cardiovascular disease - such as coronary heart disease and stroke - is another major menopause health issue that postmenopausal women face. Studies have shown that the risks quadruple about 10 years after women's final periods.3
Menopause heart disease is mainly caused by hormonal shifts and other physiological changes taking place around this life stage. With low estrogen levels, the hormone's protective effects on the heart are lost. In addition, menopause weight gain, high blood pressure, abnormal cholesterol levels, and other factors further increase the overall risk.
What Can Be Done?
Similar to osteoporosis, the best way to lower the risk of heart disease is to implement wholesome habits early on. This includes a heart-healthy menopause diet, regular exercise, addiction control, and stress relief.
Undergoing regular doctor's check-ups to monitor cholesterol levels, blood pressure, and blood sugar levels should be on every postmenopausal women's agenda.
Sexual Dysfunction

Another menopause problem almost half of all postmenopausal women face is sexual dysfunction.4 Coincidentally, it is also one of the most overlooked issues as many of its sufferers are too shy to seek adequate treatment.
Sexual dysfunction is also caused by drastic estrogen decline that leads to vaginal atrophy, or thinning of the vaginal tissue. It is characterized by vaginal dryness, irritation, and painful sex. It is also common for women to also experience loss of libido, which can put a further strain on their sex life.
What Can Be Done?
To relieve unpleasant symptoms, women can try vaginal lubricants, water-based moisturizers, and herbal gels, like those made from chamomile. Extended foreplay and frequent sex can also reduce symptoms by boosting blood flow and lubrication.
In the case natural options prove ineffective, women may also be offered several prescription medications, including low-dose vaginal estrogen preparations. However, because of potential risks, they should be used with caution.
Incontinence

Hormone-driven changes in the vulvovaginal tissue can also lead to urinary issues, like incontinence. This common menopause problem can be particularly difficult for women as it not only affects their quality of life, but also self-esteem.
In addition to experiencing an increased urge to urinate, painful urination, or accidental leakages, postmenopausal women may have more frequent urinary tract infections (about 20% in 65- to 70-year-olds and up to 50% in those above 80).5 All of those symptoms take place because lack of estrogen causes the lining of the bladder and urethra to thin.
What Can Be Done?
Managing urinary incontinence can consist of doing exercises that help strengthen the pelvic floor muscles, like Kegel exercises, as well as those that train the bladder. Maintaining a consistent urination schedule can also be beneficial.
Women with severe symptoms of urge incontinence may also consider prescription medications (such as anticholinergics), medical devices (like pessaries), or surgery (including sling procedures).
Depression

Perimenopause is when women may experience the most intense psychological menopause issues, like depression. Some of them, however, continue struggling with depression into their early postmenopause years.6
The link between menopause and depression is not well understood. Researchers believe that hormonal fluctuations play a role since estrogen is involved in the synthesis of mood-regulating neurotransmitters. Others point to aging itself, the end of fertility, the burden of menopause symptoms, and other major mid-life changes as a probable culprit.
What Can Be Done?
Menopausal depression should not be neglected. Luckily, women can find relief by eating mood-boosting foods; staying physically active; taking hormone-regulating supplements, like Macafem; and engaging in stress-relieving therapies.
Joining a support group, reaching out to friends and family, or calling free depression hotlines can also give women outlets to manage their symptoms. Also, professional help can be found through psychotherapy or prescription medications.
Key Takeaway
Thanks to medical advancements, human lifespan continues to increase. For postmenopausal women, however, this presents new challenges as they spend more years with estrogen deficiency. One of the main menopause problems is osteoporosis, which increases women's risk of fractures. Cardiovascular disease is another postmenopausal health issue women may face when they lose estrogen's heart-protective actions. Hormonal lows also affect their vulvovaginal tissues, bringing about two menopause problems: sexual dysfunction and urinary incontinence. On top of that, women may struggle with depression in early postmenopausal years due to lack of estrogen and other key changes taking place during the transition. Luckily, prevention of these postmenopausal issues is possible through regular check-ups and wholesome lifetime practices.
Sources
- American College of Obstetricians and Gynecologists. (2018). Osteoporosis. Retrieved April 8, 2021 from https://www.acog.org/womens-health/faqs/osteoporosis
- Biochemistry Research International. (2017). Elevated Cardiovascular Risks among Postmenopausal Women: A Community Based Case Control Study from Nepal. Retrieved April 8, 2021 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5433412/
- Circulation. (2020). Menopause Transition and Cardiovascular Disease Risk: Implications for Timing of Early Prevention: A Scientific Statement from the American Heart Association. Retrieved April 8, 2021 from https://www.ahajournals.org/doi/10.1161/CIR.0000000000000912
- Cleveland Clinic. (2019). Estrogen & Hormones. Retrieved April 8, 2021 from https://my.clevelandclinic.org/health/articles/16979-estrogen--hormones
- Climacteric. (2007). Menopause and cardiovascular disease: the evidence. Retrieved April 8, 2021 from https://pubmed.ncbi.nlm.nih.gov/17364594/
- Journal of Managed Care Pharmacy. (2006). Postmenopausal osteoporosis: etiology, current diagnostic strategies, and nonprescription interventions. Retrieved April 8, 2021 from https://pubmed.ncbi.nlm.nih.gov/17269852/
- Mayo Clinic. (2019). Urinary incontinence. Retrieved April 8, 2021 from https://www.mayoclinic.org/diseases-conditions/urinary-incontinence/symptoms-causes/syc-20352808
- Mayo Clinic. (2019). Vaginal atrophy. Retrieved April 8, 2021 from https://www.mayoclinic.org/diseases-conditions/vaginal-atrophy/diagnosis-treatment/drc-20352294
- Nature Reviews Disease Primers. (2016). Postmenopausal osteoporosis. Retrieved April 8, 2021 from https://www.nature.com/articles/nrdp201669
- Office on Women's Health. (2018). Menopause and your health. Retrieved April 8, 2021 from https://www.womenshealth.gov/menopause/menopause-and-your-health
- The North American Menopause Society. (n.d.). Menopause FAQs: Your Health After Menopause. Retrieved April 8, 2021 from https://www.menopause.org/for-women/menopause-faqs-your-health-after-menopause
- The North American Menopause Society. (n.d.). Urinary Incontinence. Retrieved April 8, 2021 from https://www.menopause.org/for-women/sexual-health-menopause-online/causes-of-sexual-problems/urinary-incontinence
Footnotes:
- Chronic Diseases and Translational Medicine. (2015). Primary osteoporosis in postmenopausal women. Retrieved April 8, 2021 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5643776/
- American Bone Health. (2019). How Often Should I Get Tested? Retrieved April 8, 2021 from https://americanbonehealth.org/bone-density/how-often-should-i-have-a-bone-density-test/
- American Heart Association. (2015). Menopause and Heart Disease. Retrieved April 8, 2021 from https://www.heart.org/en/health-topics/consumer-healthcare/what-is-cardiovascular-disease/menopause-and-heart-disease
- Mayo Clinic Proceedings. (2010) Vulvovaginal atrophy. Retrieved April 8, 2021 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2800285/
- Korean Journal of Urology. (2011). Urinary Tracy Infection in Postmenopausal Women. Retrieved April 8, 2021 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3246510/
- World Psychiatry. (2008). The unique challenges of managing depression in mid-life women. Retrieved April 8, 2021 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2559916/