What is Gestational Diabetes?
Diabetes during pregnancy is known as gestational diabetes. It is a type of diabetes of its own, and it differs from type 1 or type 2 diabetes mellitus in that it first appears while a woman is pregnant and disappears after delivery. In most cases, it is diagnosed between the 24th and 28th week of pregnancy.
In gestational diabetes, blood sugar levels increase and remain high causing a wide variety of physiological effects. Developing diabetes during pregnancy is quite common as up 10% of pregnant women suffer from this condition.
What Causes of Gestational Diabetes
It has not been determined yet what causes diabetes in pregnancy. In a normal progression of pregnancy, the body becomes slightly resistant to insulin, which results in higher amounts of glucose in the blood used to assemble nutrients for the developing baby. Sometimes, however, pregnancy hormones disturb insulin's function leading to abnormally high sugar levels in the blood.
Risk Factors for Gestational Diabetes
Certain factors put women at a greater risk for gestational diabetes. They include:
- Being overweight or obese
- Being 25 years of age or older
- Having polycystic ovarian syndrome
- Having a family history of type 2 diabetes
- Having had a stillbirth in previous pregnancies
- Having had a baby with marcosomia (large size)
- Being of African, Asian , Indian, Latin American, or Pacific Islander decent
Diagnosing Gestational Diabetes
Symptoms of Pregnancy Diabetes
In most cases, gestational diabetes does not produce noticeable symptoms. Some women experience very mild ones, such as increased thirst, fatigue, or more frequent urination.
Signs of Pregnancy Diabetes
Many women do not know they have gestational diabetes until they undergo a routine blood glucose test during an antenatal check-up. If the initial glucose test shows sugar levels above 140 mg/dL, your doctor will order an additional test.
Pregnancy Diabetes Tests
Gestational diabetes can be confirmed with blood tests of two kinds:
- Glucose challenge test, which involves drawing blood one hour after drinking a liquid containing glucose. Fasting is not required for this test.
- Oral glucose tolerance test, which involves multiple blood draws: the first blood sample taken after fasting for eight hours, and then three subsequent samples taken one to three hours after consuming glucose liquid.
GD is diagnosed when the results values are near at least two of the following readings:
- Fasting glucose levels: > 95 mg/dL
- After 1 hour: 180 mg/dL
- After 2 hours: 155 mg/dL
- After 3 hours: 140 mg/dL

Risks and Effects of Gestational Diabetes
Effects on the Baby
Gestational diabetes can have negative effects on the growth of the fetus:
- Babies born to mothers with pregnancy diabetes are often very big, weighing more than 9 lb (4 kg). This condition, called marcosomia, predisposes them to developing diabetes later on in life.
- Pregnancy diabetes also puts a baby at risk of being born with low glucose levels, jaundice, or respiratory distress syndrome (RDS). It can also lead to injuries during delivery, such as nerve damage.
Effects on the Mom
Women with gestational diabetes are at a higher risk of developing preeclampsia, a pregnancy complication characterized by high blood pressure and protein in the urine. Moreover, even though gestational diabetes resolves on its own in many cases, up to 50% of women develop type 2 diabetes after having a baby.
Risks and Complications of Gestational Diabetes
Delivering a large baby might warrant a cesarean section, while high glucose levels during pregnancy might result in premature birth or stillbirth.
How to Avoid Gestational Diabetes
Unfortunately, medicine currently does not offer effective strategies to avoid gestational diabetes. A wholesome diet, regular exercise as well as having a healthy weight prior to getting pregnant and preventing excess weight gain during pregnancy can significantly decrease your risk of developing it. Implementing these healthy lifestyle changes three to six months before conceiving greatly boosts your chances of succeeding.
Managing Gestational Diabetes
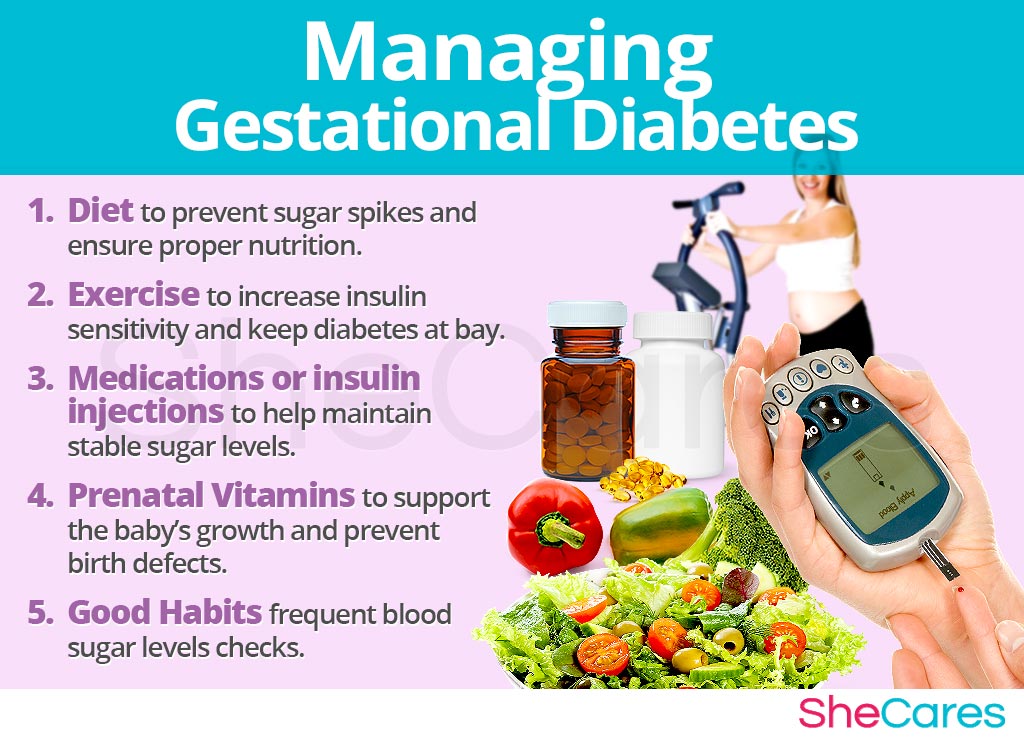
Diabetes in pregnancy guidelines might vary from woman to woman, depending on the severity of her condition and her overall health status. Although there is no treatment or cure for diabetes in pregnancy, it can be effectively managed with the following practices:
Healthy Diet
Managing gestational diabetes involves providing your body and the baby with proper nutrition by eating healthy foods that do not elevate your glucose levels. Opt for:
- Diabetes-friendly foods, such as non-starchy, low-glycemic, and whole grains options.
- Try to eat small portions every three to four hours to prevent sudden sugar spikes.
When in doubt, consult with a dietician. You might also be interested in learning how to develop a safe and effective gestational diabetes diet and meal plan.
Regular Exercise
Being physically active will help your control your sugar levels by lowering insulin resistance.
- Low-impact and relaxation-inducing exercises, such as yoga or Pilates, are safe during pregnancy. Add a few minutes of meditation or breathing exercises at the end of your workout to reduce stress.
Medications
It is important to take medications and insulin injections at proper doses to prevent low blood sugar, or hypoglycemia, which can be potentially dangerous.
Vitamins and Supplements
To complement a well-balanced diet, you should continue with:
- Prenatal vitamins as they contain a wide range of microelements, such as folic acid or iodine, necessary for the baby's development and a healthy pregnancy. Read more about prenatal vitamins.
Good Habits
- Check glucose often. Women with gestational diabetes should aim at less than 95 mg/dL before meal and less than 120 mg/dL two hours after meal.
- Read food labels. Some products contain surprisingly large amounts of added sugar.
Key Takeaways
Gestational diabetes diagnosis doesn't always come with serious complications. Many women suffering from it still have manageable pregnancies, vaginal deliveries, and healthy babies. They, however, have to be routinely tested for type 2 diabetes following the delivery. It is, therefore, particularly important to keep up with a healthy lifestyle by eating a balanced diet, exercising, and maintaining proper weight after you have your baby.
Sources
- American Diabetes Association. Gestational Diabetes. Retrieved November 8, 2017 from http://www.diabetes.org/diabetes-basics/gestational/
- American Diabetes Association. (2016). Diabetes Management Guidelines. Retrieved November 8, 2017 from http://www.ndei.org/ADA-diabetes-management-guidelines-diabetes-in-pregnancy-GDM.aspx.html
- CDC. (2017). Gestational Diabetes. Retrieved November 8, 2017 https://www.cdc.gov/diabetes/basics/gestational.html
- CDC. (2017). Gestational Diabetes and Pregnancy. Retrieved November 8, 2017 https://www.cdc.gov/pregnancy/diabetes-gestational.html
- Eunice Kennedy Shriver National Institute of Child Health and Human Development. (). Managing Gestational Diabetes. Retrieved November 8, 2017 from https://www.nichd.nih.gov/publications/pubs/Documents/managing_gestational_diabetes.pdf
- Mayo Clinic. (2015). Fetal marcosomia. Retrieved November 8, 2017 from https://www.mayoclinic.org/diseases-conditions/fetal-macrosomia/basics/definition/CON-20035423?p=1
- Mayo Clinic. (2015). Glucose tolerance test. Retrieved November 8, 2017 from https://www.mayoclinic.org/tests-procedures/glucose-tolerance-test/basics/results/prc-20014814
- Medline Plus. (2017). Gestational diabetes. Retrieved November 8, 2017 from https://medlineplus.gov/ency/article/000896.htm
- National Institute of Diabetes and Digestive and Kidney Diseases. (n.d.). Gestational Diabetes. Retrieved November 8, 2017 from https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/gestational
- The American College of Obstetricians and Gynecologists. (2013). Gestational Diabetes. Retrieved November 8, 2017 from https://www.acog.org/Patients/FAQs/Gestational-Diabetes