What is Nuchal Translucency?
A nuchal translucency ultrasound is a type of non-invasive prenatal ultrasound. It is also referred to as an NT ultrasound, NT scan, or simply nuchal translucency.
An NT scan is used to assess the risk of a baby having a genetic abnormality, like Down syndrome, Edwards syndrome, or Patau syndrome.2 It's analyzed alongside a prenatal blood test, called maternal serum screening, as part of the first trimester screening.
Nuchal translucency scan is typically performed towards the end of the first trimester, between the 11th and 13th week and 6 days or when the baby's crown-rump length (CRL) is between 45mm and 84 mm.1 If an earlier dating ultrasound was not done during the first prenatal visit, the NT scan can also be used to estimate baby's due date.
How Is A Nuchal Translucency Test Done?
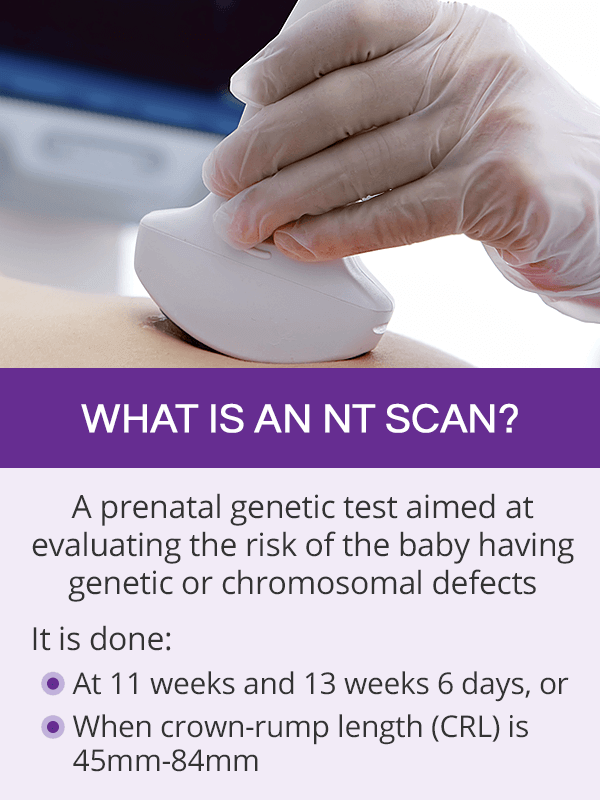
Nuchal translucency ultrasound is a safe, non-invasive, and painless prenatal test. It is performed with a full bladder in order to obtain the best quality pictures. The test should take 30-40 minutes.
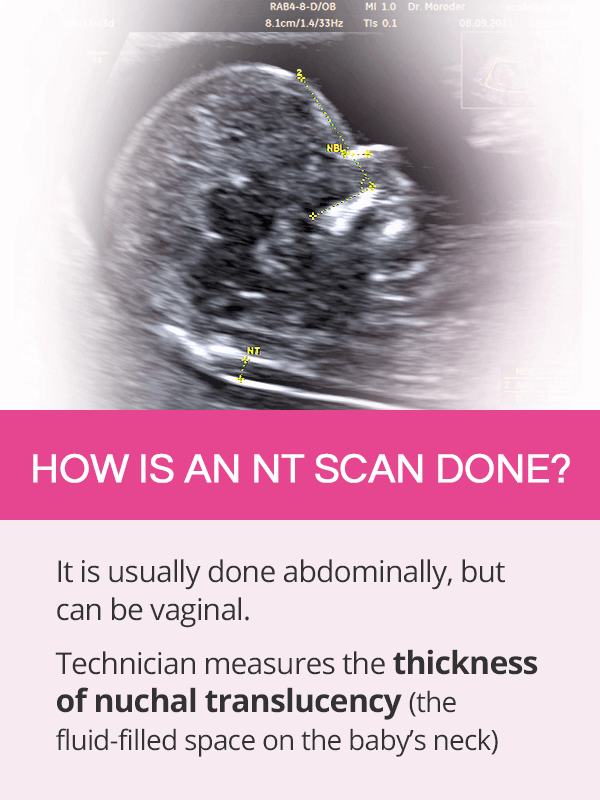
In most of the cases, NT scans are transabdominal, but sometimes a transvaginal scan is recommended. The technician will run the ultrasound transducer on a woman's belly to measure the thickness of nuchal translucency, which is the proper name for the normal, fluid-filled space at the back of the baby's neck.
If there is a risk that the baby has chromosomal or genetic defects, this area typically appears thicker on an ultrasound.
Nuchal Translucency Results
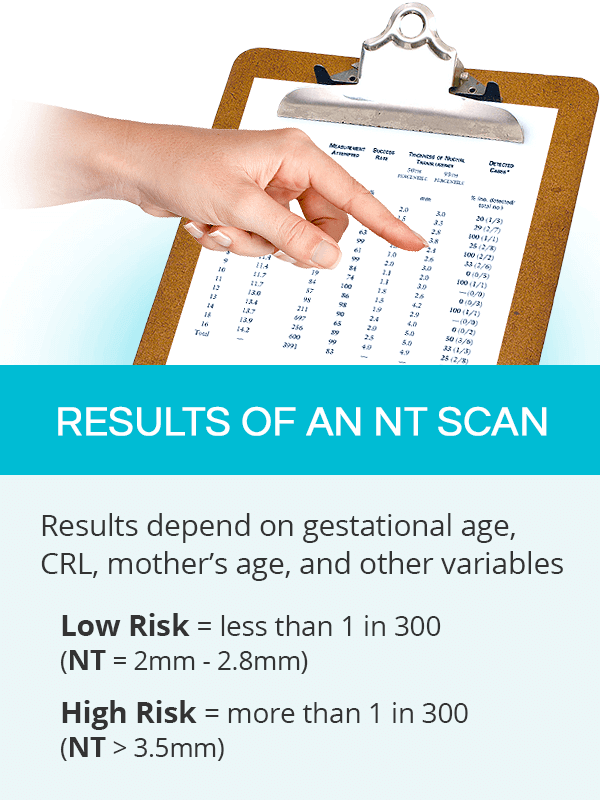
The higher the measurement for babies at the same gestational age, the higher the risk of the baby having chromosomal abnormalities and genetic disorders.
Normal Nuchal Translucency Results
Normal values of a nuchal translucency scan, which are associated with a low risk of genetic disorders, are as follows2:
- 11 weeks: up to 2mm
- 13 weeks and 6 days: up to 2.8mm
An NT scan is a time-sensitive exam as the nuchal translucency itself is no longer seen towards the end of the second trimester. As such, the results are adjusted to the baby's gestational age, CRL, maternal age, and other variables.
If the values are within the normal range, the NT scan results will say that there is a low risk (less than 1 in 300 women) that the child has defects.
Abnormal Nuchal Translucency Results
As with all screening tests, a nuchal translucency measurement higher than the normal range does not mean that the baby does have a genetic condition. It does, however, mean that there is a high risk (greater than 1 in 300 women) that she or he does.
Although the cut-off value for a normal NT has been 3.5mm, recent studies proposed a new and slightly lower value of 3.0-3.4mm as an indication for further testing, such as chromosomal microarray analysis (CMA).3
For more accuracy, nuchal translucency results are analyzed together with the maternal serum screening results. If abnormal, they are usually followed by more invasive diagnostic prenatal tests, such as chorionic villus sampling (CVS) or amniocentesis, which will be used to confirm or rule out the suspected defects.
Nuchal Translucency Cost
The exact nuchal translucency's cost is difficult to estimate as it depends on individual insurance coverage.
Some insurance companies consider it a part of routine prenatal care, while others only cover it partially. In that case, the patient will be responsible for her co-insurance or deductible according to her specific policy.
Nuchal translucency's cost without insurance can range from $400-500 or more, not including the blood work that is performed as part of the first trimester screening.
Key Takeaways
Nuchal translucency ultrasound, also called an NT scan, is an important prenatal test aimed at evaluating the risk of a baby having chromosomal abnormalities or genetic conditions. It can only be performed between the 11th and 13th week and 6 days or when the baby's crown-rump length (CRL) is between 45mm and 84 mm. It is a time-sensitive test as the nuchal translucency, the fluid-filled space on the back of the baby's neck, is not visible later on as the pregnancy progresses. The NT scan is usually done on the lower abdomen, although it can be done through the vagina. Because it is a screening test, the results can only evaluate the risk of the baby having genetic defects. For a full diagnosis, more invasive follow-up tests, like amniocentesis, will be recommended in the case of high risk results.
Sources
- International Journal of Computer Science and Information Security. (2009). Measurement of Nuchal Translucency Thickness for Detection of Chromosomal Abnormalities using First Trimester Ultrasound Fetal images. Retrieved August 20, 2019 from https://arxiv.org/ftp/arxiv/papers/1001/1001.1986.pdf
- Journal of Research in Medical Sciences. (2015). Normal reference range of fetal nuchal translucency thickness in pregnant women in the first trimester, one center study. Retrieved August 20, 2019 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4746871/
- Journal of Clinical & Diagnostic Research. (2013). The Associations of Nuchal Translucency and Fetal Abnormalities; Significance and Implications. Retrieved August 20, 2019 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3681077/
- National Health Service. (2018). NHS Fetal Anomaly Screening Programme Handbook. Retrieved August 20, 2019 from https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/749742/NHS_fetal_anomaly_screening_programme_handbook_FINAL1.2_18.10.18.pdf
- The Fetal Medicine Foundation. (n.d.). Nuchal translucency assessment. Retrieved August 20, 2019 from https://fetalmedicine.org/research/assess/nt
Footnotes:
- Pregnancy, Birth & Baby. (2018). Nuchal translucency scan. Retrieved August 20, 2019 from https://www.pregnancybirthbaby.org.au/nuchal-translucency-scan
- Medline Plus. (2018). Nuchal translucency test. Retrieved August 20, 2019 from https://medlineplus.gov/ency/article/007561.htm
- Ultrasound in Obstetrician and Gynecology. (2017). Cut-off value of nuchal translucency as indication for chromosomal microarray analysis. Retrieved August 20, 2019 from https://obgyn.onlinelibrary.wiley.com/doi/full/10.1002/uog.17421