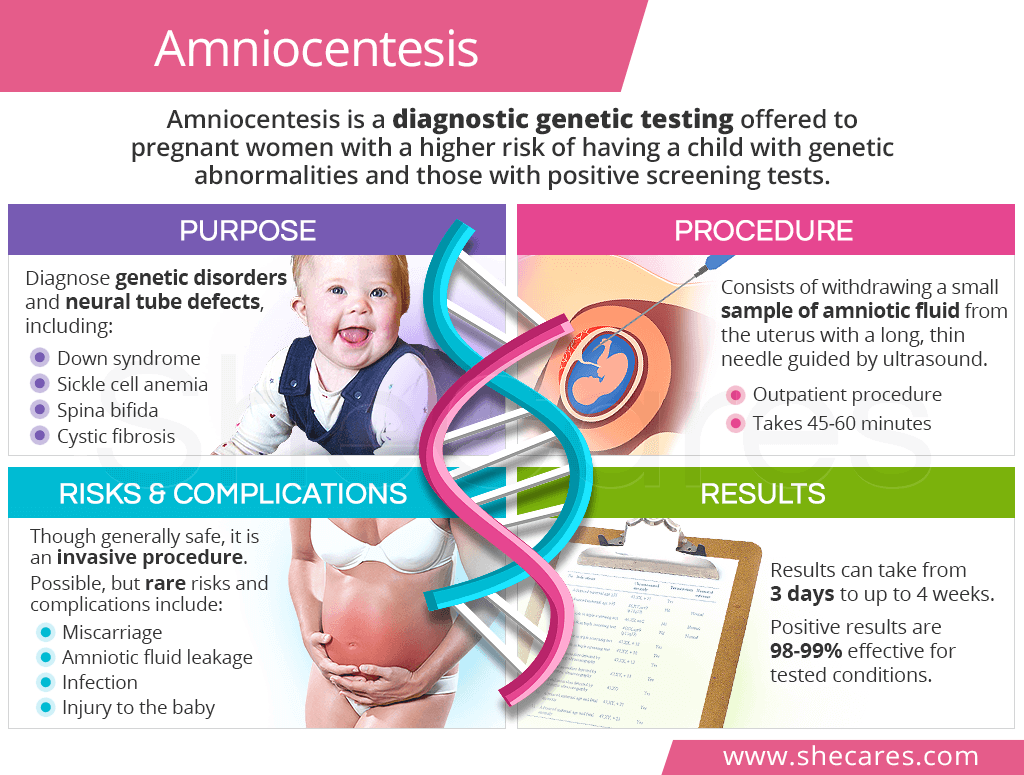
What is Amniocentesis?
An amniocentesis is a type of diagnostic prenatal genetic testing, typically offered to pregnant women between the 15th and 20th week. It consists of taking a sample of amniotic fluid, which surrounds the fetus, and testing it for genetic abnormalities.
As opposed to genetic screening tests, which only evaluate the risk of the fetus having a genetic abnormality, diagnostic genetic tests during pregnancy confirm or rule out whether she or he actually has it.
Purpose of Amniocentesis
An amniocentesis test allows for a detection of chromosomal abnormalities, gene mutations, and neural tube defects, which could lead to genetic disorders and birth defects, including:
- Down syndrome
- Edwards syndrome
- Patau syndrome
- Cystic fibrosis
- Tay-Sachs disease
- Thalassemia
- Sickle cell anemia
- Fragile X syndrome
- Congenital heart defects
- Anencephaly
Besides serving as genetic testing, amniocentesis can also be used in late pregnancy to diagnose fetal lung disease and infections as well as perform a paternity test and drain excess amniotic fluid from the womb.
Who Needs an Amniocentesis?
Amniocentesis for genetic make-up is generally offered to pregnant women in two circumstances: when prenatal genetic screening tests showed positive results or when a woman has certain risk factors for having a baby with genetic abnormalities, such as:
- Advanced age
- Chronic conditions, like high blood pressure, lupus, epilepsy, or diabetes
- History of miscarriages or having a child with birth defects
- Family history of genetic disorders
- Being a carrier of or having a partner who is carrier of a genetic disorder
- Certain ethnicity associated with a higher risk of some genetic disorders
In all cases, undergoing an amniocentesis is entirely a woman's choice since it is not a mandatory, routine exam.
Amniocentesis Procedure
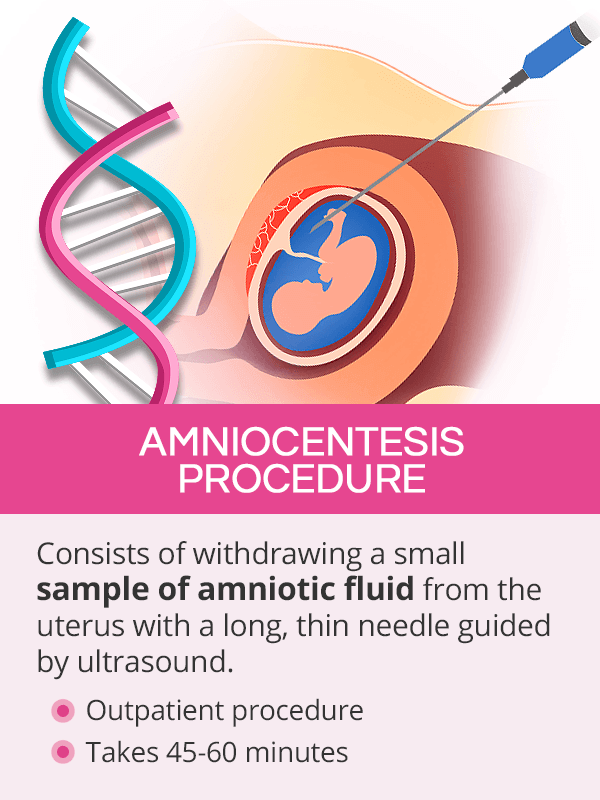
An amniocentesis procedure is typically done on an outpatient basis, which means a woman will be discharged home the same day. It takes about 45-60 minutes.
During the procedure, the position of the baby will first be located with ultrasound before a long, thin needle is inserted into the uterus through the abdomen. Once a small sample of amniotic fluid is withdrawn, the needle can be removed and the procedure is completed. Through all the steps, the baby is monitored to ensure his or her safety and well-being.
Women generally do not report excessive pain or other discomforts during or after amniocentesis. Following the procedure, a woman is advised to avoid heavy lifting, strenuous exercise, and sexual activity for two days.
Amniocentesis Risks & Complications

Amniocentesis is generally a safe procedure. However, as an invasive diagnostic genetic testing, it carries certain post-procedure risks that should be considered before making the decision to undergo one.
Possible amniocentesis risks and complications include the following:
Miscarriage. Post-amniocentesis miscarriage risk is small, up to 0.3%, when done in the second trimester.1
Amniotic fluid leakage. About 1% of women might have vaginal leakage of the fluid, which resolves itself within two days in the majority of cases without causing further complications.2
Rh sensitization. In rare cases, fetal cells enter the mother's bloodstream, which is not a problem unless a woman is Rh negative, and the baby is Rh positive. It may trigger a reaction of her immune system to attack the fetal red blood cells. An injection of anti-D immunoglobulin after the procedure can help prevent this complication.
Infection. An infection in the uterus is also a rare, but a possible complication of amniocentesis.In some cases, it might trigger a miscarriage.
Injury to the baby. Perhaps the most feared amniocentesis complication by the mothers, an injury to the baby is very rare. Precautions are taken to avoid touching the baby and the placenta with the needle.
Severe cramping, fever, vaginal bleeding or fluid discharge, redness at the insertion site, or changes in fetal movement should be immediately reported to a doctor.
Amniocentesis Results
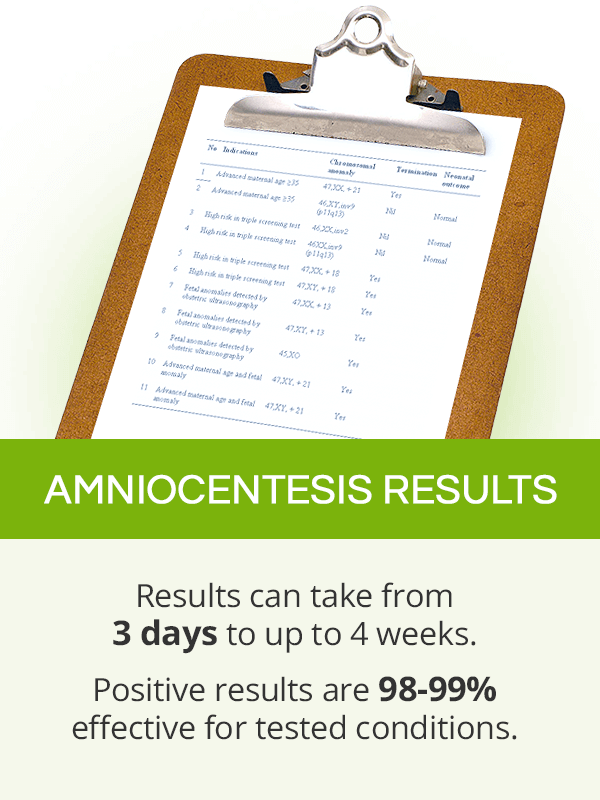
It might take up to two to four weeks to obtain full amniocentesis results, although some parts might be ready within three days.
Analyzing the Results
A woman will analyze the results of amniocentesis with her OBGYN or - in some cases - a genetic specialist. It is important to understand that though effective in detecting a number of genetic conditions and birth defects (98-99% accuracy), an amniocentesis does not test for all existing genetic abnormalities, neither their severity.3 It is possible to obtain negative results and still have a child with another genetic abnormality that was not tested for.
Making Important Decisions
In the case of treatable genetic abnormalities, like spina bifida, a surgery during pregnancy or right after birth will be suggested. When a baby is diagnosed with an untreatable genetic condition, such as Down syndrome, couples usually contemplate one of the following options:
Key Takeaways
Amniocentesis is a known cause of concerns among expectant mothers as it is associated with the risk of pregnancy loss. Although it is true that this invasive diagnostic test during pregnancy carries a 1% risk of miscarriage, an amniocentesis is generally a safe and relatively painless procedure that can be an important in tool in monitoring fetal well-being, especially in women with known risk factors for having a child with genetic disorders or positive screening tests. Done between the 15th and 20th week of pregnancy, an amniocentesis procedure involves using a needle to take a sample of amniotic fluid from the uterus and testing it for genetic conditions and birth defects, like Down syndrome, spine bifida, or cystic fibrosis. Though optional, undergoing amniocentesis gives couples time to come to terms with the results, weigh their options, and make the best choices for their future.
Sources
- Better Health Channel. (n.d.). Pregnancy Tests: Amniocentesis. Retrieved July 10, 2019 from https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/pregnancy-tests-amniocentesis
- Israel Journal of Health Policy Research. (2016). How can we improve amniocentesis decision-making? Retrieved July 10, 2019 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4743405/
- Medline Plus. (2019). Amniocentesis. Retrieved July 10, 2019 from https://medlineplus.gov/ency/article/003921.htm
- National Health Service. (2019). Amniocentesis. Retrieved July 10, 2019 from https://www.nhs.uk/conditions/amniocentesis/results/
- Planned Parenthood. (n.d.). What's amniocentesis? Retrieved July 10, 2019 from https://www.plannedparenthood.org/learn/pregnancy/prenatal-care/whats-amniocentesis
- Royal College of Obstetricians and Gynaecologists. (2011). Chorionic villus sampling and amniocentesis. Retrieved July 10, 2019 from https://www.rcog.org.uk/globalassets/documents/patients/patient-information-leaflets/pregnancy/pi-chorionic-villus-sampling-and-amniocentesis.pdf
Footnotes:
- Mayo Clinic. (2020). Amniocentesis. Retrieved August 8, 2022 from https://www.mayoclinic.org/tests-procedures/amniocentesis/about/pac-20392914
- Obstetrics & Gynecology. (2021). Clinical significance of persistent amniotic fluid leakage after genetic amniocentesis. Retrieved August 8, 2022 from https://obgyn.onlinelibrary.wiley.com/doi/abs/10.1002/pd.1970060104
- Cleveland Clinic. (22). Amniocentesis. Retrieved August 8, 2022 from https://my.clevelandclinic.org/health/treatments/4206-genetic-amniocentesis