What is Rh Incompatibility?
Rh incompatibility is a condition that happens when an Rh-negative woman is exposed to an Rh-positive blood. It usually occurs either during pregnancy or blood transfusion.
Being Rh-positive means that one's red blood cells contain a protein, called an Rh-factor. Conversely, being Rh-negative means that the Rh factor is absent. Both scenarios do not have any consequences on one's general health. However, potentially serious complications might arise during pregnancy when a mother who is Rh-negative carries a baby that is Rh-positive.
What is Rh Sensitization?
If an Rh-positive baby's blood crosses to Rh-negative mother's blood circulation, her immune system can undergo Rh sensitization, which involves treating the baby's blood as a foreign substance and developing antibodies to attack it. Research shows that less than 20% of Rh-negative women Rh sensitize.
In the majority of cases, this immune system's reaction occurs at the time of delivery. So, most firstborn babies are not affected because there is not enough time for the antibodies to cross over to the baby's circulatory system. The risks increase only slightly with the second pregnancy and then rise significantly with subsequent pregnancies with the Rh-positive fetuses as there are already Rh antibodies present in maternal blood.
Signs and Symptoms of Rh Incompatibility
The mother shows no physical symptoms of Rh disease. About 50% of babies born from a rhesus disease pregnancy have mild symptoms that can be successfully treated. Those more severely affected might exhibit the following signs and symptoms:
- Lethargy
- Low muscle tone
- Enlarged spleen, liver, or heart
- Fluid build-up in body cavities
- Pale skin
- Jaundice
- Poor feeding
- Fast breathing
Causes and Risk Factors for Rh Incompatibility
Rh incompatibility is caused by the contact of Rh-negative maternal blood with Rh-positive fetal blood. So, risk factors for this condition include instances in which that contact might have occurred, such as:
Previous pregnancy
External cephalic version
Bleeding during pregnancy
Trauma to the abdomen during pregnancy
History of miscarriage, ectopic pregnancy, or an abortion
History of amniocentesis or chorionic villus sampling
Effects of Rh Incompatibility on Pregnancy
Rh incompatibility is not harmful to the mother; it can, however, be very dangerous to the baby before birth as well as after delivery. Its effects vary from mild to severe and might lead to a range of serious complications:
Hemolytic anemia, which results from the destruction of the baby's red blood cells.
Hyperbilirubinemia, which is excess bilirubin, also occurs from red blood cell breakdown.
Kernicterus, a type of brain damage, which can cause movement problems, low muscle tone, or mental retardation.
Hydrops fetals, a condition which might result in heart failure, fluid build-up in the body, and even stillbirth.
Risks and Complications
Severe cases of Rh disease might result in fetal death in utero or an emergency premature delivery.
Rh Incompatibility Tests
Most women are diagnosed as Rh-negative during the initial prenatal visit, which is when a woman's blood is tested for its type and the presence of the Rh factor.
Blood tests, such as Coombs' test, and an ultrasound might be ordered throughout pregnancy to verify whether fetal blood has crossed into maternal circulation as well as to detect Rh disease antibodies in the maternal blood. They can also be used to screen for signs of potential complications, such as fetal anemia.
Prevention of Rh Incompatibility
Rhesus incompatibility complications can be prevented with early detection. Rh-negative mothers are given an injection of Rh immunoglobulin, also called RhoGAM, which prevents Rh sensitization to fetal blood and the immune system's attack on the baby's blood.
This preventive shot is safe for the baby and is normally given to Rh-negative women around the 28th week of gestation and then shortly after delivery. Women who suffered a miscarriage, had an abortion, or an amniocentesis should receive this shot as well.
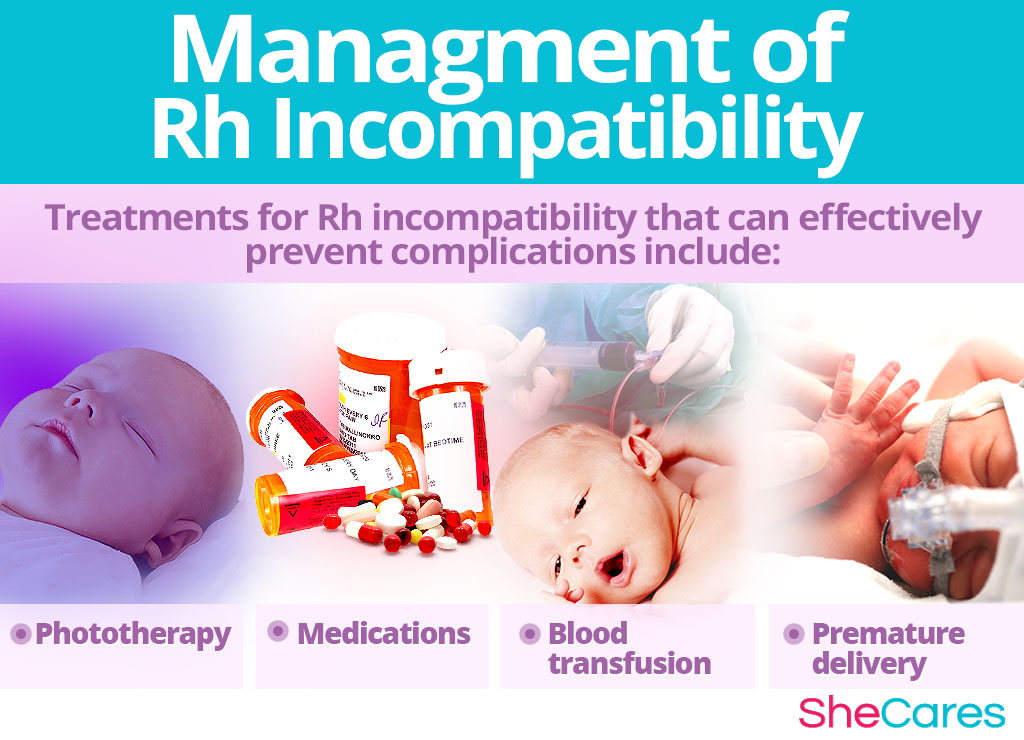
Management of Rh Incompatibility
Treatment of rhesus incompatibility depends on its severity, and it might be started before or right after delivery. They include:
- Phototherapy uses light to reduce the amount of bilirubin through the process of photo-oxidation.
- Medications, such as intravenous immunoglobulin, prevents the destruction of red blood cells, thus lowering the levels of bilirubin.
- Blood transfusions can be done while the baby is still in the womb or after birth. They are meant to remove excess bilirubin and antibodies from the baby's blood.
- Sometimes, a premature delivery after the 34th week is necessary to start proper treatment and prevent further complications.
Key Takeaways
To this day, prevention is the most effective approach to reducing the risk of potentially serious complications of Rh disease. Undergoing regular prenatal visits can enable you to get promptly diagnosed and adequately treated so you can bring your baby safely to term. It can also ensure that your subsequent pregnancies proceed without complications and result in healthy babies.
Sources
- March of Dimes. (n.d.). Rh disease. Retrieved January 15, 2018 from https://www.marchofdimes.org/complications/rh-disease.aspx
- Medline Plus. (2017). Rh Incompatibility. Retrieved January 10, 2018 from https://medlineplus.gov/ency/article/001600.htm
- National Heart, Lung, and Blood Institute. (n.d.). Rh Incompatibility. Retrieved January 10, 2018 from https://www.nhlbi.nih.gov/health-topics/rh-incompatibility
- NHS. (2018). Rhesus disease. Retrieved January 15, 2018 from http://www.winchesterhospital.org/health-library/article?id=11595
- The American College of Obstetricians and Gynecologists. (2013). The Rh Factor: How It Can Affect Your Pregnancy? Retrieved January 15, 2018 from https://www.acog.org/Patients/FAQs/The-Rh-Factor-How-It-Can-Affect-Your-Pregnancy
- The Embryo Project Encyclopedia. (2011). Rh Incompatibility in Pregnancy. Retrieved January 15, 2018 from https://embryo.asu.edu/pages/rh-incompatibility-pregnancy
- Stanford Children's Health. (n.d.). Rh disease. Retrieved January 15, 2018 from http://www.stanfordchildrens.org/en/topic/default?id=rh-disease-90-P02498
- University of Rochester. (n.d.). Rh Disease. Retrieved January 15, 2018 from https://www.urmc.rochester.edu/encyclopedia/content.aspx?ContentTypeID=90&ContentID=P02498
- US Department of Health and Human Services. (n.d.). Rh Incompatibility. Retrieved January 15, 2018 from https://healthfinder.gov/FindServices/SearchContext.aspx?topic=14706&show=1
